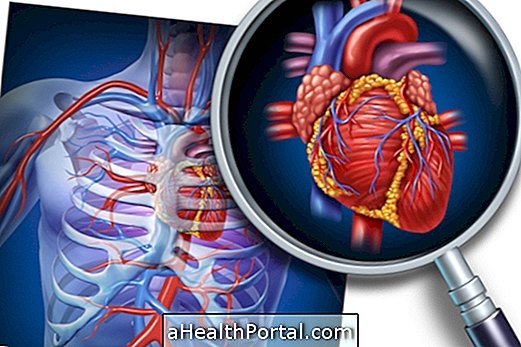
Cardiac amyloidosis also known as hard heart syndrome is a rare, very serious disease that affects the heart muscle due to the accumulation of proteins called amyloid on the heart walls.
This disease is more common in men over 40 years of age and causes signs of heart failure, such as easy tiredness and difficulty climbing stairs or performing small efforts.
Protein accumulation can occur only in the atrial septum, as it is more common in the elderly, or in the ventricles, and may cause heart failure.

Symptoms
Symptoms of cardiac amyloidosis may be:
- Intense urge to urinate during the night;
- Enlargement of the veins of the neck, scientifically called jugular stasis;
- Heart palpitations;
- Accumulation of fluid in the lungs;
- Liver enlargement;
- Low pressure when lifting a chair, for example;
- Fatigue;
- Persistent dry cough;
- Weight loss with no apparent cause, no diet or exercise increase;
- Intolerance to physical effort;
- Fainting spells;
- Shortness of breath;
- Swollen legs;
- Swollen abdomen.
Amyloidase in the heart is characterized by excess proteins in the heart muscle and can be caused by a multiple myeloma, have a family origin or can arise with advancing age.
How to know if it is Cardiac Amyloidosis
There is usually no suspicion of this disease on a first visit, so it is common for physicians to order multiple tests to detect other diseases before arriving at the diagnosis of cardiac amyloidosis.
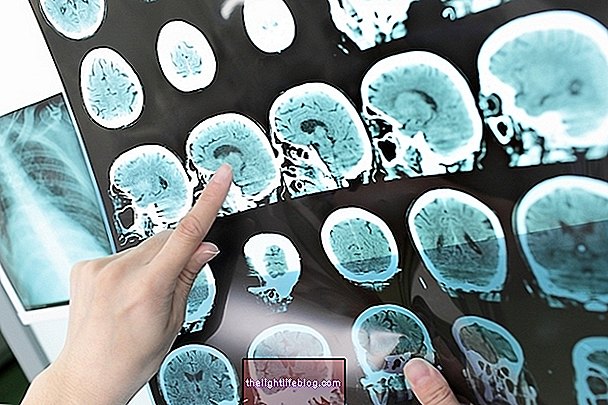
The diagnosis is made through the observation of symptoms and through examinations requested by the cardiologist, such as electrocardiogram, echocardiogram and magnetic resonance imaging, which may detect cardiac arrhythmias, alterations in the heart's functions and disturbances in the electrical conduction of the heart, but the diagnosis of cardiac amyloidosis can only be proven through a biopsy of the cardiac tissue.
This diagnosis can be reached when the ventricular wall thickness is above 12 mm and when the person does not present high blood pressure, but has one of the following characteristics: atrial dilatation, pericardial effusion or heart failure.
Treatment
For the treatment can be used diuretic and vasodilator drugs that ameliorate the symptoms of the disease. The use of pacemakers and automatic defibrillators can be used as alternatives for the control of the disease and in the most serious cases, the most indicated treatment is heart transplantation. See the risks and how to recover from heart transplantation by clicking here.
Depending on the severity of the disease, anticoagulants may be used to prevent clots from forming in the heart, reducing the likelihood of strokes. Chemotherapy may be used when the cause of cardiac amyloidosis is multiple myeloma
The person should avoid salt, prefer diuretic foods and avoid making efforts to save the heart. The family should also avoid giving bad news because intense emotions can lead to important heart changes that can lead to heart attack.
See all types and symptoms caused by Amyloidosis.
Possible Complications of Cardiac Amyloidosis
Complications related to cardiac amyloidosis involve severe cardiac changes such as cardiac conduction disorder, restrictive cardiomyopathy, low cardiac output and isolated atrial impairment.
Cardiac amyloidosis is a progressive disease that has a very poor prognosis. Familial type cardiac amyloidosis has a more conservative prognosis and can lead to sudden death. The senile form that develops with advancing age may result in severe restrictive cardiomyopathy, with a high risk of death or may result only in isolated atrial involvement, leading to arrhythmia such as atrial fibrillation.