Systemic epidermal necrolysis, or NET, is a rare skin disease characterized by the presence of lesions throughout the body that can lead to permanent skin peeling. This disease is mainly caused by the use of medicines like Allopurinol and Carbamazepine, but can also be the result of bacterial or viral infections, for example.
NET is painful and can be fatal in up to 30% of cases, so as soon as the first symptoms appear, it is important to see a dermatologist so that the diagnosis can be confirmed and treatment started.
The treatment is performed in the Intensive Care Unit and is done mainly with the suspension of the medicine that is causing the disease. In addition, due to exposure of the skin and mucosa, preventive measures are taken to avoid hospital infections, which may further compromise the patient's clinical condition.

Symptoms of NET
The most characteristic symptom of toxic epidermal necrolysis is the skin lesion in more than 30% of the body that can bleed secrete liquids, favoring dehydration and infections.
The main symptoms are similar to a flu, such as:
- Malaise;
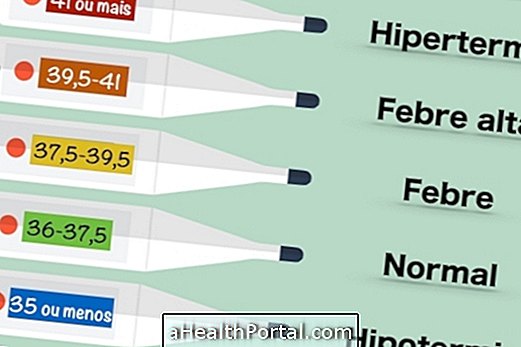
- High fever;
- Cough;
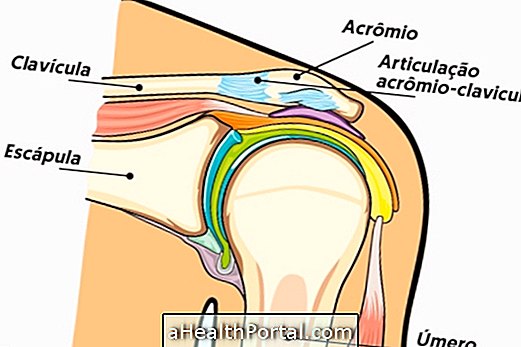
- Muscle and joint pain.
These symptoms, however, disappear after 2 to 3 days and are followed by:
- Skin rashes, which may bleed and be painful;
- Areas of necrosis around the lesions;
- Desquamation of the skin;
- Emergence of bubbles;
- Alteration in the digestive system due to the presence of mucosal lesions;
- Sore mouth, throat, and anus ulcers, less often;
- Swelling of the eyes.
The lesions of toxic epidermal necrolysis occur throughout the body, unlike Stevens-Johnson syndrome, which despite having the same clinical manifestations, diagnosis and treatment, lesions are more concentrated in the trunk, face and chest. Learn more about Stevens-Johnson Syndrome.
Main causes
Toxic epidermal necrolysis is mainly caused by medications, such as Allopurinol, Sulfonamide, anticonvulsants or antiepileptics, such as Carbamazepine, Phenytoin and Phenobarbital, for example. In addition, people who have autoimmune diseases, such as Systemic Lupus Erythematosus, or have compromised immune systems, such as AIDS, are more likely to have skin lesions characteristic of necrolysis.
In addition to being caused by medications, skin lesions can occur due to infections by viruses, fungi, protozoa or bacteria and the presence of tumors. This disease can also be influenced by advanced age and genetic factors.

How is the treatment done?
The treatment of toxic epidermal necrolysis is done in the intensive care unit of burns and consists of the elimination of the medicine that is being used by the patient, since normally NET is the result of adverse reactions to certain drugs.
In addition, fluid and electrolyte replacement is lost due to extensive skin lesions by injecting serum into the vein. Daily care of the lesions by a nurse is also performed to avoid skin or generalized infections, which can be very serious and compromise the health of the patient.
When the lesions reach the mucosa, food can become difficult for the person and, therefore, food is administered intravenously until the mucous membranes are recovered.
To lessen the discomfort caused by the injuries can also be made compresses of cold water or use of neutral creams that promote hydration of the skin. In addition, your doctor may also recommend the use of anti-allergies, steroids, or antibiotics, for example if NET is caused by bacteria or if the patient has acquired an infection as a consequence of the disease and may worsen the clinical picture.
How is the diagnosis made?
The diagnosis is made based mainly on the characteristics of the lesions. There is no laboratory test that can indicate which drug is responsible for the disease and the stimulus tests are not indicated in this case, as it may cause a worsening of the disease. Thus, it is important that the person informs the doctor if they have any disease or if they use any medication, so that the doctor can confirm the diagnosis of the disease and identify the causative agent.
In addition, to confirm the diagnosis, the doctor usually asks for skin biopsy, blood count, microbiological blood tests, urine and wound secretion to check for any infection, and the dosage of some factors responsible for the immune response.