Essential thrombocythemia, or ET, is a hematological disease characterized by increased platelet concentration in the blood, which increases the risk of thrombosis and bleeding.
This disease is usually asymptomatic and discovered only after a routine blood count. However, the diagnosis is only confirmed by the physician after excluding other possible causes of platelet enlargement, such as iron deficiency anemia, for example.
Treatment is usually done with medications that can reduce the number of platelets in the blood and decrease the risk of thrombosis, and should be used as directed by the general practitioner or hematologist.
Main symptoms
Essential thrombocythemia is usually asymptomatic and is only seen after the blood count, for example. However, it can result in some symptoms, the main ones being:
- Feeling of burning in the feet and hands;
- Splenomegaly, which is enlargement of the spleen;
- Chest pain;
- Sweating;
- Weakness;
- Headache;
- Transient blindness, which may be partial or complete;
- Weight loss.
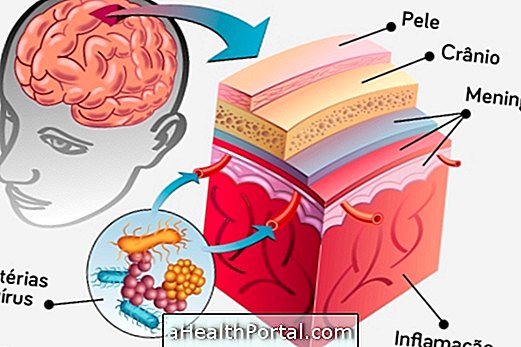
In addition, people diagnosed with essential thrombocythemia are at increased risk of thrombosis and bleeding. This disease is more common to occur in people over 60, but can also happen in people under 40 years.
Is Essential Thrombocythemia Cancer?
Essential thrombocythemia is not cancer, since there is no proliferation of malignant cells, but rather normal cells, in this case, of platelets, characterizing the platelet or thrombocytosis. This disease remains stable for about 10 to 20 years and has a low rate of leukemic transformation, less than 5%.

How is the diagnosis made?
The diagnosis is made by the general practitioner or hematologist according to the signs and symptoms presented by the patient, in addition to the results of the laboratory tests. It is also important to rule out other causes of platelet enlargement, such as inflammatory diseases, myelodysplasia and iron deficiency, for example. Know the main causes of platelet enlargement.
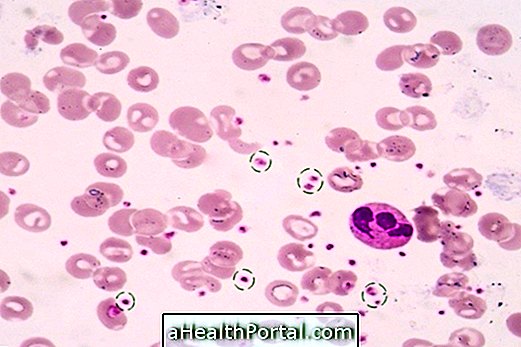
The laboratory diagnosis of essential thrombocythemia is done initially by means of a blood count analysis, in which the increase in platelets is observed, with a value above 450, 000 platelets / mm³ of blood. Recurrence of platelet concentration on different days is usually done to check if the value remains increased.
If plaquetosis is sustained, genetic tests are performed to check for the presence of a mutation that may be indicative of essential thrombocythemia, the JAK2 V617F mutation, which is present in more than 50% of patients. If the presence of this mutation is verified, it is necessary to exclude the occurrence of other malignancies and verify the nutritional reserves of iron.
In some cases, bone marrow biopsy may be performed, where an increase in the concentration of megakaryocytes, which are the precursor blood cells of platelets, may be observed.
Treatment for essential thrombocythemia
Treatment for essential thrombocythemia is aimed at reducing the risk of thrombosis and bleeding, and it is generally recommended by the doctor to use medicines to decrease the amount of platelets in the blood, such as Anagrelide and Hydroxyurea, for example.
Hydroxyurea is the medicine commonly recommended for people considered to be at high risk, ie they are over 60 years old, have had an episode of thrombosis and have a platelet count higher than 1500000 / mm³ of blood. However, this medicine has some side effects, such as hyperpigmentation of the skin, nausea and vomiting.
The treatment of patients characterized as low risk, who are those under 40 years, is usually made with acetylsalicylic acid according to the guidance of the general practitioner or hematologist.
In addition, in order to reduce the risk of thrombosis, it is important to avoid smoking and treat possible underlying diseases, such as hypertension, obesity and diabetes, as they increase the risk of thrombosis. Learn what to do to prevent thrombosis.