Diabetic foot is a term used to refer to the increased risk that diabetics have of presenting foot problems such as sores, thrombosis, infections and ulcers. However, this type of problem is only more common when the disease is not well controlled, and is characterized by symptoms such as tingling and burning in the feet.
Thus, ideally, all diabetics, in addition to having proper treatment, should try to prevent foot problems, taking care to wear comfortable shoes and do not remove calluses, and seek medical attention as soon as there is a change in the feet.
What symptoms help identify

The main symptoms of this problem include:
- Loss of sensation in feet;
- Frequent tingling sensation;
- Burning in the feet and ankles;
- Pain and feeling of needles;
- Numbness in feet;
- Weakness in the legs.
Despite the presence of symptoms, most diabetics only realize the severity of the problem when a wound or infection does not pass.
How is the treatment done?
The treatment of diabetic foot is done according to the type of foot injury and its severity and should always be guided by a doctor, even in the case of small cuts or wounds, as they can worsen rapidly.
Thus, the treatment may involve:
- Take antibiotic medicines;
- Use antimicrobial ointments at the affected site;
- Controlling diabetes from changes in diet, use of medication and insulin;
- Change daily the dressing of the wound, according to the doctor's or nurse's instructions;
- Avoid pressing the affected area, avoiding to wear closed shoes or leave the foot in the same position for a long time.
In more severe cases, surgery may be necessary to remove the affected region of the skin and promote healing. However, when the wound is not detected soon or when the patient does not follow the treatment properly, it may be necessary to amputate the foot or part of the foot.
5 care to avoid serious complications
The following are 5 tips to avoid the main problems that affect the foot of the diabetic:
1. Maintain controlled blood glucose

This is the most important step to avoid diabetic foot because when sugar levels remain high for a long time, blood has more difficulty reaching the ends of the body, and the feet are the region most affected by poor circulation.
Thus, when there is little blood reaching to the feet, the cells become weak and the foot begins to lose sensitivity, causing cuts or wounds to heal very slowly and only to be noticed when they are at a very advanced stage.
2. Watch your feet daily

Because of the risk of loss of sensation, diabetics should have a habit of evaluating their feet daily, whether at bath or when waking up, for example. If the physical condition does not allow or if the visibility is not good, you can use a mirror or ask for help from another person during the inspection of the feet.
Check for cracks, chilblains, cuts, wounds, calluses, or changes in color. Call your health care provider if you notice any of these changes.
3. Keep feet clean and moisturized

You should wash your feet every day with warm water and mild soap, being careful to sanitize well between the toes and the heel. Then you should dry your feet with a soft towel, without rubbing the skin, just drying with slight pressures of the towel.
After washing, it is still important to pass an odorless moisturizer all over the foot, being careful not to leave cream accumulated between the fingers and nails. It should be allowed to dry naturally before wearing socks or closed shoes.
4. Cut the nails 2 times a month and do not remove calluses

It is important to avoid fingernails very often, and it is ideal to do only 2 times a month, so as not to stimulate the appearance of nail corners or ingrown nails. In addition, you should avoid removing the cuticle because it is important to protect the skin from wounds and scratches.
It is also important to cut the nails in a straight line, and calluses should only be removed by a foot specialist and be aware of the presence of diabetes. If the calluses appear too often, talk to the doctor to investigate the causes and start treatment.
5. Wear tight, closed shoes

The ideal shoe for the diabetic should be closed, to avoid sores and cracks, besides being soft, comfortable and with rigid soles, to give safety during the walk.
Women should prefer low heels and squares, which provide a better balance for the body. One should avoid plastic footwear, thin-pointed or tight, and a good tip is to always have a second pair of shoes to change in the middle of the day, so that the foot does not suffer the pressure and discomfort of the same shoe for a long time .
It is important to remember that in the presence of any changes in the feet or lack of sensitivity, the doctor should be sought for treatment to be started soon, and that the best way to prevent diabetic foot is to control blood glucose through proper nutrition.
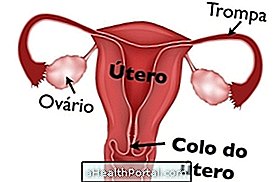
In addition to foot problems, the diabetic also has higher risks of having genital infections.