Malaria is an infectious disease transmitted through the bite of the female Anopheles mosquito, which transmits a protozoan of the Plasmodium family. In this way, the best form of prevention consists of measures to avoid being bitten, through the use of repellent and protections in the windows, for example.
Once in the organism of the affected person, these parasites go to the liver, where they multiply and then reach the bloodstream, where they invade and rupture red blood cells, causing symptoms such as fever, sweating, chills, nausea, vomiting, headache and weakness.
Malaria has a cure, but it is important that treatment be started quickly, since in many cases the disease can become severe, with anemia, decreased platelets, renal failure or, even, brain impairment, in which the chances of complications and death are much greater.

Main symptoms
The first symptoms of malaria usually appear between 8 and 14 days after transmission, which can take up to 30 days or more. The most common symptoms include:
- Fever, which may arise and disappear in cycles;
- Sweating and chills;
- Strong headache;
- Nausea and vomiting;
- Muscle pain throughout the body;
- Weakness and constant tiredness;
- Yellowish skin and eye.
Most of these symptoms can be difficult to identify as a sign of malaria, so if they arise it is important to go to the doctor to diagnose the disease and initiate appropriate treatment, especially if you are in a place where malaria is frequent, such as in Amazon region and Africa, for example.
In addition, these symptoms can appear in cycles, that is, manifest every 48 hours or 72 hours, depending on the species of Plasmodium that is infecting the body. This happens because of their life cycle, as they develop, reproduce and fall into the bloodstream.
The most serious form of malaria occurs when the infection engulfs the brain, causing headache, neck stiffness, seizures, drowsiness, and coma. Other complications include anemia, platelet reduction, renal failure, and respiratory failure. Learn more about the symptoms of malaria and cerebral malaria.
How Transmission Happens
Malaria transmission occurs through the bite of the female infected Anopheles mosquito, which acquired the parasite by stinging a person infected with the disease. It is important to remember that malaria is not contagious, that is, it is not transmitted from person to person, except in rare cases of syringe sharing, poorly controlled transfusion or childbirth.
Generally, the mosquito bites people during dusk or dusk. The most at risk of contamination are South America, Central America, Africa and part of Asia, especially in places with clean water with little current, humidity and temperature between 20º and 30ºC. In Brazil, the states most affected by malaria are Amazonas, Roraima, Acre, Tocantins, Pará, Amapá, Mato Grosso, Maranhão and Rondônia.
Cycle of malaria infection

The cycle of the Plasmodium parasite in the human body happens as follows:
- The bite of the female of the mosquito Anopheles transmits, through its saliva, the Plasmondium to the bloodstream of the person, in its Sporozoite phase;
- The sporozoites travel atheistic liver, where they mature and multiply, for about 15 days, giving rise to the form of Merozoites;
- The Merozoites break the liver cells and reach the bloodstream, invading the red blood cells;
- Inside the infected blood cells, which are called Schizonts, the parasites multiply and break this cell, and begin to invade others, in a cycle that lasts from 48 to 72 hours.
Within each schizont, the cycle is variable according to the Plasmodium species, being 48 hours for the species P. falciparum, P. vivax, and P. ovale and 72 h for P. malariae . During the period that the schizonts are ruptured, the symptoms may be accentuated, especially fever and chills.
How to confirm the diagnosis
After the first symptoms appear, it is recommended to go to the hospital or the emergency room, especially if the symptoms appear every 48 to 72 hours. In this way, the doctor can identify the presence of the parasite in the body through blood tests, such as thickens or immunological tests, and can start the appropriate treatment, preventing the infection from worsening and life-threatening.
How is the treatment done?
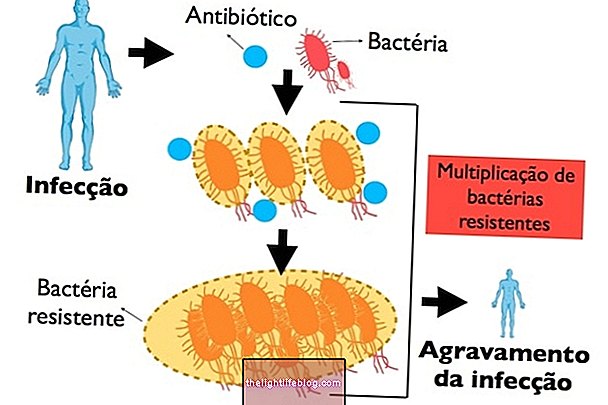
Malaria treatment is done with antimalarial medicines such as Chloroquine, Primaquine, Artemeter and Lumefantrine or Artesunato and Mefloquinta, for example, which act by destroying Plasmodium and preventing its transmission.
The medications chosen, doses and duration are indicated by the doctor according to the age, severity of the disease and analysis of health conditions. Children, infants and pregnant women need a special treatment with Quinine or Clindamycin, always in accordance with the medical recommendations and, generally, hospitalization is indicated.
It is also recommended:
- Feed normally;
- Do not consume alcoholic beverages;
- Do not stop the treatment before medical advice, even if the symptoms disappear before, by the risk of relapse and complications of the disease.
Treatment of malaria should be started as soon as possible, as it can progress in a severe way and, without appropriate treatment, can lead to death. Learn more about how treatment is done to recover faster.
How to protect yourself
Prevention of malaria can be done through:
- Wear light-colored clothing and thin fabric with long sleeves and long pants;
- Avoid areas prone to contamination of the disease, especially during dusk or dawn, for example;
- Use DEET-based repellent (NN-diethylmetatoluamide), respecting manufacturer's directions for repellent replacement;
- Put mosquito screens on windows and doors;
- Avoid lakes, ponds and rivers in the late afternoon and evening .
Those who travel to a place where there are cases of malaria can receive a preventive treatment, called chemoprophylaxis, with anti-malarial drugs such as Doxycycline, Mefloquine or Chloroquine, for example.
However these drugs have strong side effects, so the doctor usually indicates this type of prevention for people who are at greater risk of developing serious illness, such as going to places with high rates of transmission or when the person has some disease that may have major complications with the infection.
These medicines should only be used after medical advice and are usually started 1 day before the trip and persist for a few days or weeks after returning.