Scleroderma is a chronic autoimmune disease that causes excessive production of collagen, leading to hardening of the skin and affecting joints, muscles, blood vessels and some internal organs such as the lungs and heart.
This disease mainly affects women over 30 years, but it can also occur in men and children, and is divided into two types, localized and systemic scleroderma, according to their intensity. Scleroderma has no cure and its treatment is done to alleviate symptoms and slow the progression of the disease.
Localized Scleroderma
Localized scleroderma, formerly called CREST syndrome, is characterized by red spots that appear on the skin and may stiffen over time, or disappear.
This type of disease mainly affects the hands and face, and the changes usually only reach the skin and the muscles, being rare to spread through the body and affect the internal organs.

Systemic scleroderma
Systemic scleroderma is characterized by affecting the skin, muscles, blood vessels and internal organs such as heart, lungs, kidneys and intestines.
The symptoms of scleroderma depend on the affected regions, but usually begin with thickening and swelling of the fingertips.

Symptoms of scleroderma
The main symptoms of scleroderma are:
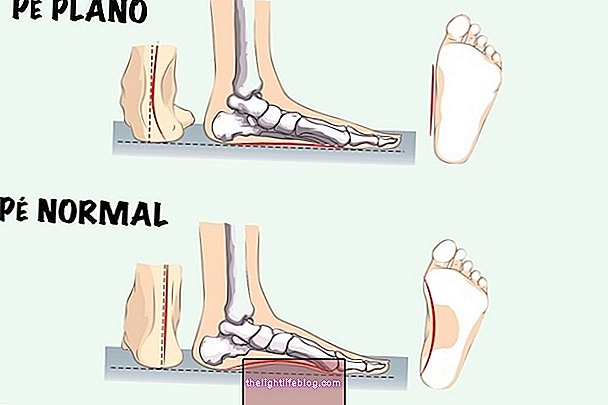
- Thickening and stiffness of the skin;
- Constant swelling of fingers and toes;
- Darkening of the fingers in cold places or during episodes of excessive stress;
- Constant itching in the affected region;
- Loss of hair;
- Very dark and very light spots on the skin.
The first manifestations of the disease begin in the hands and after months or years pass to the face, leaving the skin hardened, without elasticity and without wrinkles, which also makes it difficult to open the mouth completely.
Complications of scleroderma
The main complications of scleroderma are:
- Difficulty in wiggling fingers;
- Difficulty swallowing;
- Difficulty breathing;
- Anemia;
- Arterial hypertension;
- Liver inflammation;
- Arthritis;
- Heart problems such as inflammation and heart attack;
- Renal insufficiency.
These complications appear after years of development of the disease, and occur mainly in the systemic form of the disease.
Diagnosis of scleroderma
The diagnosis of scleroderma is made based on the symptoms and clinical manifestations of the skin, but in some cases it can be difficult to correctly identify this disease, as it evolves slowly and its first symptoms are similar to other skin problems.
The doctor may also order biopsy from the affected region and perform tests such as CT and MRI scans to assess whether internal organs have also been affected.
Treatment of scleroderma
Scleroderma has no cure and its treatment is done to reduce the patient's symptoms according to the organs and regions of the body affected, which may include:
- Remedies to control high blood pressure, such as Atenolol or Nifedipine;
- Anti-inflammatory medicines such as Ketoprofen or Ibuprofen;
- Remedies to weaken the immune system, such as D-penicillamine or interferon-alpha, to try to prevent the progression of the disease;
- Corticosteroids, such as Cortisone or Betamethasone, to reduce pain and inflammation;
- Remedies to improve the functioning of the heart, such as Digoxin;
- Physiotherapy to improve breathing and increase flexibility of joints.
The treatment for scleroderma must be adapted by the physician according to the individual, since there is no cure for scleroderma.