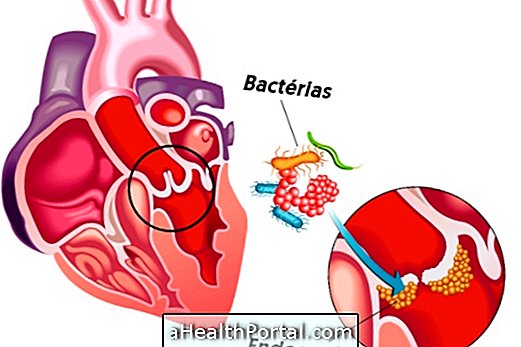
Endocarditis is inflammation of the tissue lining the inside of the heart, especially the heart valves. It is usually caused by an infection in another part of the body that spreads through the blood until it reaches the heart and can therefore also be known as infective endocarditis.
Because it is often caused by bacteria, endocarditis is usually treated with the use of antibiotics administered directly into the vein. However, if you have another cause, endocarditis can also be treated with antifungals or just anti-inflammatory drugs to relieve discomfort. Depending on the severity of the symptoms, you may still be advised to be admitted to the hospital.
See how the treatment of bacterial endocarditis is done.
Main symptoms
Symptoms of endocarditis may appear slowly over time and therefore are often not easy to identify. The most common include:
- Persistent fever and chills;
- Excessive sweating and general malaise;
- Pale skin;
- Pain in muscles and joints;
- Nausea and decreased appetite;
- Swollen feet and legs;
- Persistent coughing and shortness of breath.
In rare cases, other symptoms such as weight loss, the presence of blood in the urine and increased sensitivity to the left side of the abdomen over the spleen may still occur.
However, these symptoms can vary greatly especially according to the cause of endocarditis. So whenever a heart problem is suspected, it is very important to consult a cardiologist quickly or go to the hospital for diagnostic tests such as the electrocardiogram and confirm that there is a problem that needs treatment.
See 12 other symptoms that may indicate a heart problem.
How to confirm the diagnosis
The diagnosis of endocarditis can be made by a cardiologist. Typically, evaluation begins with evaluation of symptoms and auscultation of heart function, but it is also necessary to do some diagnostic tests such as echocardiogram, electrocardiogram, chest x-ray, and blood tests.
Possible Causes of Endocarditis
The main cause of endocarditis is infection by bacteria, which may be present in the body due to an infection elsewhere in the body, such as a tooth or a skin wound, for example. When the immune system is unable to fight off these bacteria, they can spread through the blood and reach the heart, causing inflammation.
Thus, as bacteria, fungi and viruses can also affect the heart, resulting in an endocarditis, however, the treatment is done differently. Some of the most common ways to develop endocarditis include:
- Have mouth sores or an infection in the tooth;
- Catch a sexually transmitted disease;
- Having an infected wound on the skin;
- Use a contaminated needle;
- Use a urinary catheter for a long time.
Not everyone develops endocarditis, because the immune system is able to fight most of these microorganisms, however, the elderly, children or people with autoimmune diseases are at greater risk.

Main types of endocarditis
The types of endocarditis are related to the cause that originated and are classified in:
- Infective endocarditis: when it is caused by the entry of bacteria into the heart or fungi in the body, causing infections;
- Non-infectious endocarditis or endocarditis marantica: when it arises as a consequence of several problems, such as cancer, rheumatic fever or autoimmune diseases.
Regarding infectious endocarditis, which is the most common, when it is caused by bacteria, it has the name of bacterial endocarditis, when it is caused by fungi is called fungal endocarditis.
When it is caused by rheumatic fever it has the name of rheumatic endocarditis and when it is caused by lupus it is called endocarditis of Libman Sacks.
How is the treatment done?
Treatment for endocarditis is by intravenous antibiotics or antifungals for at least 4 to 6 weeks. To relieve the symptoms, are prescribed anti-inflammatories, fever remedies and, in some cases, corticosteroids.
In cases where destruction of the heart valve by the infection occurs, surgery may be necessary to replace the valve damaged by a prosthesis that may be biological or metallic.
Untreated endocarditis can lead to complications such as heart failure, stroke, stroke, pulmonary embolism, or kidney problems that may progress to acute renal failure.