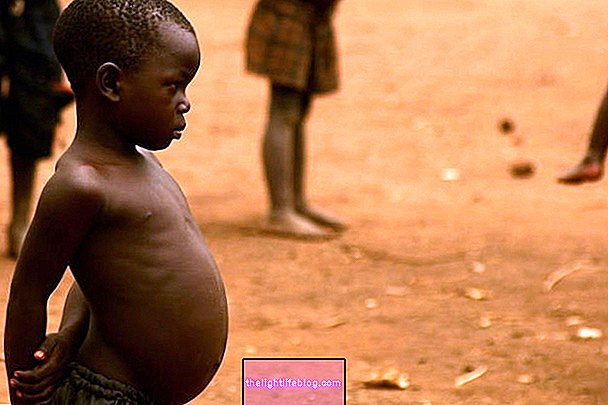
Rhabdomyosarcoma is a type of cancer that develops in soft tissues, affecting mainly children and adolescents up to 18 years of age. This type of cancer can appear in almost all parts of the body, since it develops where there is skeletal muscle, however, it can also appear in some organs such as the bladder, prostate or vagina.
Normally, rhabdomyosarcoma is formed during pregnancy, even during the embryonic phase, in which the cells that will give rise to the skeletal muscle become malignant and begin to multiply without control, causing cancer.
Rhabdomyosarcoma is curable when diagnosis and treatment are carried out in the early stages of tumor development, with a greater likelihood of cure when treatment is started soon after the child's birth.

Types of radiomyosarcoma
There are two main types of rhabdomyosarcoma:
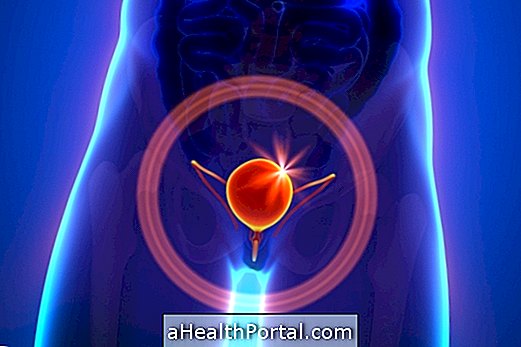
- Embryonic rhabdomyosarcoma, which is the most common type of this cancer and occurs most frequently in babies and children. Embryonic rhabdomyosarcoma tends to develop in the area of the head, neck, bladder, vagina, prostate and testicles;
- Alveolar rhabdomyosarcoma, which occurs most often in older children and adolescents, affecting mainly muscles of the chest, arms and legs. This cancer gets its name because the tumor cells form small hollow spaces in the muscles, called alveoli.
In addition, when rhabdomyosarcoma develops in the testicles, it becomes known as paratesticular rhabdomyosarcoma, being more common in people up to 20 years of age and usually leads to swelling and pain in the testicle. Know other causes of swelling in the testicles
Symptoms of rhabdomyosarcoma
The symptoms of rhabdomyosarcoma vary according to the size and location of the tumor, which may be:
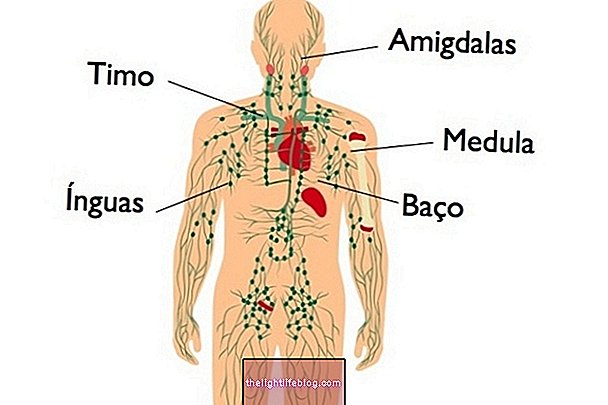
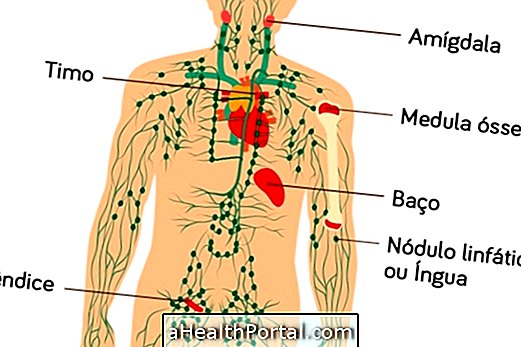
- Mass that can be seen or felt in the region in the limbs, head, trunk or groin;
- Tingling, numbness and pain in the limbs;
- Constant headache;
- Bleeding from the nose, throat, vagina or rectum;
- Vomiting, abdominal pain and intestinal constipation, in the case of tumors in the abdomen;
- Yellowed eyes and skin, in the case of tumors in the bile ducts;
- Bone pain, cough, weakness and weight loss, when rhabdomyosarcoma is at a more advanced stage.
The diagnosis of rhabdomyosarcoma is carried out through blood and urine tests, X-rays, computed tomography, magnetic resonance imaging and tumor biopsy to check for the presence of cancer cells and to identify the degree of malignancy of the tumor. The prognosis of rhabdomyosarcoma varies from person to person, however the sooner the diagnosis is made and treatment begins, the greater the chances of cure and the lesser the possibility of the tumor to reappear in adulthood.
How the treatment is done
The treatment of rhabdomyosarcoma should be started as soon as possible, being recommended by the general practitioner or pediatrician, in the case of children and adolescents. Usually, surgery to remove the tumor is indicated, especially when the disease has not yet reached other organs.
In addition, chemotherapy and radiation therapy can also be used before or after surgery to try to reduce the size of the tumor and eliminate possible metastases in the body.
The treatment of rhabdomyosarcoma, when performed in children or adolescents, can have some effects on growth and development, causing lung problems, delays in bone growth, changes in sexual development, infertility or learning problems.
Was this information helpful?
Yes No
Your opinion is important! Write here how we can improve our text:
Any questions? Click here to be answered.
Email in which you want to receive a reply:
Check the confirmation email we sent you.
Your name:
Reason for visit:
--- Choose your reason --- DiseaseLive betterHelp another personGain knowledge
Are you a health professional?
NoMedicalPharmaceuticalsNurseNutritionistBiomedicalPhysiotherapistBeauticianOther
Bibliography
- INCA. Rhabdomyosarcoma - version for Health Professionals. Available in: . Accessed on 25 May 2020
- Moretti, Giovana. et al. Head and neck rhabdomyosarcoma: 24 cases and literature review. Braz. j. otorhinolaryngol. (Impr.). v. 76, n. 4. p. 533-537, 2010. Available from.
- HOLCOMB III, G.W. et al. Ashcraft: Pediatric Surgery. 6th ed. Rio de Janeiro: Elsevier, 2017. pp. 743-751.