Hyperparathyroidism is a disease that causes the exerted production of the hormone PTH, released by the parathyroid glands, which are located in the neck behind the thyroid.
The hormone PTH helps to maintain calcium levels in the blood and for this, its main effects include reabsorption of calcium in the kidneys, greater absorption of calcium from the diet in the intestine, as well as the removal of calcium stored in the bones to release in the bloodstream.
Hyperparathyroidism can arise in 3 ways:
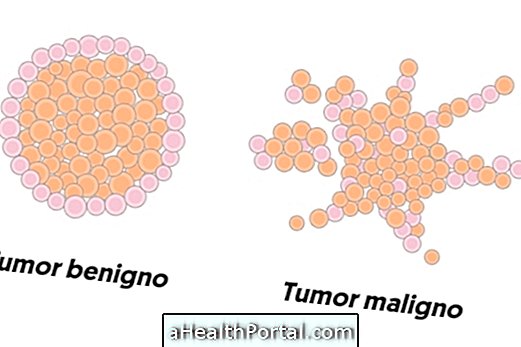
- Primary hyperparathyroidism : occurs when a disease of the parathyroid itself causes a hypersecretion of the hormone pTH, mainly due to an adenoma or hyperplasia of these glands ;:
- Secondary hyperparathyroidism : arises due to a disorder in the body's metabolism, which stimulates parathyroid hormones, especially due to renal failure, which causes a decrease in the levels of calcium and phosphorus in the circulation;
- Tertiary hyperparathyroidism : it is more rare, and arises after some time of secondary hyperparathyroidism, when the parathyroidals start to secrete more PTH on their own.
When identified, hyperparathyroidism needs to be promptly treated as it may have negative consequences, such as weakening of bones, increasing the risk of fractures. In addition, excess calcium in the blood can still cause changes in the functioning of muscles, kidney stones, increased blood pressure and other cardiovascular problems.
This disease is cured when surgery is performed to remove the gland, however, before that, remedies can be indicated that can be used to control the symptoms.

Main symptoms
Some of the most common signs and symptoms in cases of hyperparathyroidism are:
- Bone fragile and at greater risk of fractures;
- Muscle weakness;
- Development of kidney stones;
- Increased urge to urinate;
- Constant pain in the belly;
- Excessive tiredness;
- Memory problems;
- Nausea, vomiting and loss of appetite.
Hyperparathyroidism does not always cause symptoms, especially in the earliest stages, so it is common for this disease to be identified in routine blood tests that show changes in blood calcium levels.
How to diagnose
The diagnosis of hyperparathyroidism is made with the dosage of the hormone PTH, which is increased in all types of the disease. Then the endocrinologist will ask for other tests that help identify the cause of the problem, such as calcium dosage, which is elevated in primary and reduced secondary hyperparathyroidism, and tests such as calcium and phosphorus in the urine, for example.
X-ray examinations can also help identify the disease because it shows bones with demineralization and osteoporosis. In more advanced cases, this examination may show the formation of excavations and proliferation of tissues and vessels in the bones, which is known as "brown tumor".
In addition, imaging of the neck region with ultrasound, scintigraphy, or MRI, for example, may help identify changes in parathyroid glands.
How is the treatment done?
The first step in the treatment of primary hyperparathyroidism is the correction of calcium levels that, if they are greatly altered, may be the main cause of the symptoms. For this, there are a few different options, which include hormone replacement, made especially in women after menopause, because the replacement of some hormones helps to maintain calcium levels in the bones. Bisphosphonates also help increase calcium deposition in the bones by lowering free calcium in the blood. Check out other causes of excess calcium in the blood and how to treat it.
Surgery may also be indicated in the case of primary hyperparathyroidism, as it removes the affected glands, curing the disease. However, it has some risks such as nerve damage that controls the vocal chords or a marked decrease in calcium levels.
In the case of secondary hyperparathyroidism, it is necessary to do the correct monitoring and treatment of renal insufficiency, restoration of levels of vitamin D and calcium, which are diminished. Calcimimetic remedies have a calcium-like effect, causing the glands to produce fewer hormones. An example of these remedies is cinacalcete.