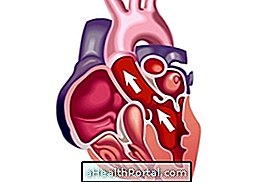
Aortic stenosis is heart disease characterized by a narrowing of the aortic valve, which makes it difficult to pump blood to the body, resulting in a feeling of shortness of breath, chest pain and palpitations.
This disease is mainly caused by aging and its more severe form can lead to sudden death, however, when diagnosed early, it can be treated with medication and, in severe cases, by surgery to replace the aortic valve. Find out about recovery after heart surgery.
Aortic stenosis is a heart disease where the aortic valve is narrower than normal, making it difficult to pump blood from the heart to the body. This disease is mainly caused by aging and its more severe form can lead to sudden death, but when diagnosed in time it can be treated through surgery to replace the aortic valve.

Main symptoms
The symptoms of aortic stenosis arise mainly in the severe form of the disease and are usually:
- Sensation of shortness of breath when performing physical exercises;
- Chest tightening that gets worse over the years;
- Chest pain that worsens when exerting effort;
- Fainting, weakness or dizziness, especially when performing physical exercises;
- Heart palpitations.
The diagnosis of aortic stenosis is made through clinical examination with the cardiologist and complementary exams such as chest x-ray, echocardiogram or cardiac catheterization. These tests, in addition to identifying changes in the functioning of the heart, also indicate the cause and severity of aortic stenosis.
The treatment of aortic stenosis is done through surgery, in which the deficient valve is replaced by a new valve, which may be artificial or natural, when it is made from swine or bovine tissue. Replacing the valve will cause the blood to be properly pumped from the heart to the rest of the body, and the symptoms of tiredness and pain will disappear. Without surgery, patients with severe or symptomatic aortic stenosis survive on average 2 years.
How is the treatment done?
The treatment of aortic stenosis depends on the stage of the disease. When there are no symptoms, and the disease has been discovered through examinations there is no need for specific treatment. However, after the onset of symptoms, the only form of treatment is aortic valve replacement surgery, where the defective valve is replaced by a new valve, normalizing the distribution of blood through the body. This surgery is indicated mainly for patients who have severe aortic stenosis, since the mortality rate is high. Here are the treatment options:
1. In people without symptoms
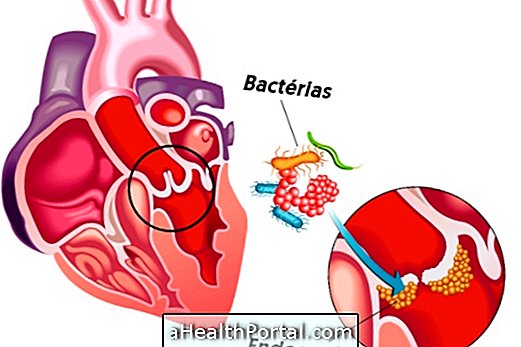
The treatment for people who do not have symptoms is not always done with surgery. It can be done with the use of medications and changes in lifestyle, such as avoiding competitive sports and professional activities that require intense physical effort. The drugs used in this phase can be:
- To avoid infective endocarditis;
- To treat diseases associated with aortic stenosis.
Patients who do not present symptoms that may be indicated for surgery if they have a very reduced valve, progressive reduction of cardiac function or increased changes in cardiac structure.
2. In people with symptoms
Initially, diuretics such as Furosemide can be used to control symptoms, but the only effective treatment for people who have symptoms is surgery, since the drugs are no longer sufficient to control the disease. There are two procedures for the treatment of aortic stenosis, depending on the state of health of the patient:
- Valve replacement by surgery: standard open chest surgery procedure so the surgeon can reach the heart. The defective valve is removed and a new valve is placed.
- Replacement of the valve by catheter: known as TAVI or TAVR, in this procedure the defective valve is not withdrawn and the new valve is implanted over the old one, from a catheter placed in the femoral artery, in the thigh, or from a cut done close to the heart.
Valve replacement per catheter is usually performed on patients with greater disease severity and less ability to overcome open chest surgery.
Types of Valve for Replacement
There are two types of valve for replacement in open chest surgery:
- Mechanical valves: are made of synthetic material and have greater durability. They are usually used in patients under 60 years of age, and after their implantation the person will have to take daily anticoagulant medications and do periodic blood tests for the rest of his life.
- Biological valves: Made from animal or human tissue, they last from 10 to 20 years, and are usually recommended for patients over 65 years. In general, you do not need to take anticoagulants, unless you have other problems that need this type of medicine.
The choice of the valve is made between the doctor and the patient, and depends on the age, the lifestyle and the clinical picture of each one.

Risks and complications that may occur during surgery
The risks that aortic valve replacement surgery presents are:
- Bleeding;
- Infection;
- Formation of thrombi that can clog blood vessels causing, for example, stroke;
- Infarction;
- New valve defects placed;
- Need for new operation;
- Death.
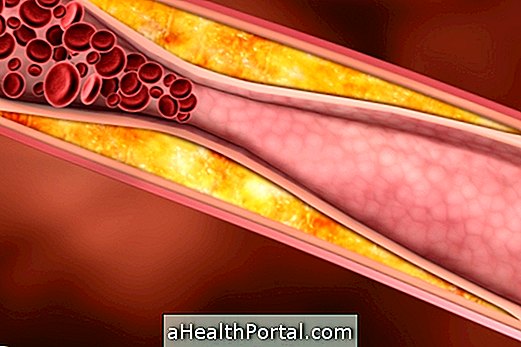
Risks depend on factors such as age, severity of heart failure and the presence of other diseases, such as atherosclerosis. In addition, being in a hospital environment also carries risks of complications such as pneumonia and hospital infection. Understand what hospital infection is.
The catheter replacement procedure in general carries fewer risks than conventional surgery, but there is a greater chance of stroke, one of the causes of stroke.
What happens if you do not treat aortic stenosis?
Untreated aortic stenosis can progress with worsening of cardiac function and symptoms of severe tiredness, pain, dizziness, fainting, and sudden death. From the appearance of the first symptoms, the life expectancy may be only 2 years, in some cases, so it is important to consult the cardiologist to verify the need for surgery and subsequent performance of the same. See how recovery is after aortic valve replacement.
Main causes
The main cause of aortic stenosis is age: over the years, the aortic valve undergoes changes in its structure, which is followed by calcium accumulation and inadequate functioning. Symptoms usually begin after age 65, but the person may not feel anything until they eventually pass away without knowing that they have aortic stenosis.
In younger people, the most common cause is rheumatic disease, where aortic valve calcification also occurs, and symptoms begin to appear around age 50. Other more rare causes are congenital defects such as the bicuspid aortic valve, systemic lupus erythematosus, high cholesterol and rheumatoid disease. Understand what rheumatism is.