Hospital infection is defined as any infection acquired while the person is hospitalized, and may still manifest during hospitalization or after discharge, as long as it is related to hospitalization or hospital procedures.
Acquiring an infection in the hospital is not uncommon, as this is an environment where many people are sick and on antibiotics. During the period in a hospital, some of the major factors that cause the infection are:
- Imbalance of the bacterial flora of the skin and of the organism, usually due to the use of antibiotics;
- Drop in the defense of the immune system of the hospitalized person, as much by the illness, as by the use of medicines;
- Performing invasive procedures such as catheter passage, passage of probes, biopsies, endoscopies or surgeries, for example, that break the barrier of protection of the skin.
Generally, the microorganisms that cause the hospital infection do not cause infections in other situations because they take advantage of the environment with few harmless bacteria and the drop in resistance of the patient to settle. In spite of this, hospital bacteria often develop serious and difficult to treat infections, as they are more resistant to antibiotics, so in general, it is necessary to use more potent antibiotics to cure this type of infection.

How is the control performed?
In Brazil, the Ministry of Health and Anvisa determine that every environment for health care has certain care to prevent hospital infection. In the hospital, there should be a Hospital Infection Control Commission (CCIH), made up of a group of health professionals, such as doctors and nurses, who are responsible for studying the sources and causes of to reduce the number of infections.
The important activities of the CCIH can be divided into:
- Development of standards and routines for cleaning and disinfecting environments, establishing frequency, type of disinfectant, especially in critical areas such as nurseries, surgical centers or ICUs, for example;
- Determination of rules for patients, visitors and professionals, to reduce the risk of infections, such as limiting the number of visitors, establishing standards and training for hygiene, collecting exams, applying medications, dressing or preparing food, for example ;
- Stimulation of hygiene measures, mainly of the hands, that are of the main vehicles of transmission of microorganisms, with the frequent washing, or with the use of alcohol gel;
- Guidelines for the correct use of antibiotics, preventing them from being prescribed improperly, and increasing the proliferation of resistant bacteria;
- Guidance on the use of chemicals to eliminate micro-organisms, such as germicides, disinfectants, antiseptics, cleaning agents;
- Carry out the surveillance of cases of infection, to understand the causes and to elaborate forms of prevention.
To decrease the infection rate of a hospital, basic care should be taken with all patients regardless of their diagnosis and treatment performed.
In addition, it is important to encourage hospital discharge whenever possible, avoiding long hospital stays, as the chances of infection increase over time.
Types of hospital infection
The hospital infection can be acquired in several places of the body, being the most common types are:
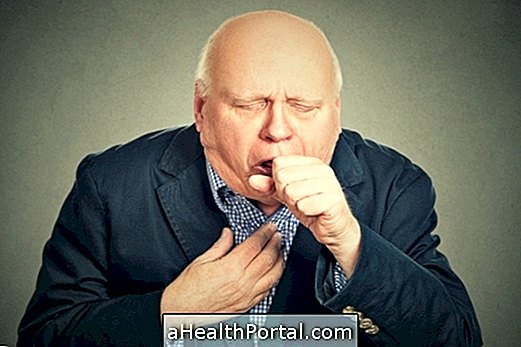
1. Pneumonia
Hospital-acquired pneumonia is usually severe, and more common in people who are bedridden, dehydrated, or who have difficulty swallowing, because of the risk of aspiration of food or saliva. Some common bacteria in this type of pneumonia are Klebsiella, Enterobacter, Pseudomonas, Acinetobacter, Staphylococcus aureus, Legionella, Mycoplasma, plus some types of virus.
- Symptoms : pain in the chest, cough with yellowish or bloody discharge, fever, tiredness, lack of appetite and shortness of breath.
2. Urinary tract infection
Hospital urinary tract infection is facilitated by the use of catheter during the period of hospitalization, although anyone can develop it. Some of the most involved bacteria in this situation include Proteus sp, Pseudomonas aeruginosa, Klebsiella sp., Enterobacter sp., Enterococcus faecalis and fungi, such as Candida.
- Symptoms : pain or burning on urination, abdominal pain, bleeding from the urine, fever.

3. Skin infection
Skin infections are very common due to the applications of injections and venous accesses to medications or collections of exams, surgery or biopsy scar or the formation of bedsores. Some of the microorganisms involved in this type of infection are Staphylococcus aureus, Enterococcus Klebsiella, E. Proteus, Enterobacter sp, Serratia sp, Streptococcus sp, Staphylococcus aureus or Staphylococcus epidermitis, for example.
- Symptoms : There may be an area of redness and swelling on the skin, with or without the presence of blisters. Generally, the site is painful and hot, and there may be purulent and foul smelling secretions.
4. Blood infection
Infection of the bloodstream is called septicemia, and usually arises after infection from a part of the body that spreads through the bloodstream. This type of infection is severe, and if not quickly treated can quickly cause organ failure and death risk. Any of the microorganisms of the infections can spread through the blood, and some of the most common are E. coli , Staphylococcus aureus, Staphylococcus epidermitis or Candida, for example.
- Symptoms : fever, chills, pressure drop, weak heartbeat, drowsiness.
There are also a number of other less common types of nosocomial infections that affect various regions of the body such as the oral cavity, digestive tract, genitals, eyes or ears, for example. Any hospital infection should be identified quickly and treated with potent antibiotics to prevent it becoming severe and life threatening to the person, so in the presence of any signs or symptoms of this situation should be reported to the doctor in charge.
Some of these bacteria may develop resistance to the vast majority of antibiotics and are known as superbugs. Learn how the use of inappropriate antibiotics are the source of the superbugs and how to treat them.
Who has more risk
Anyone can develop a hospital infection, however, those with a greater fragility of immunity are at greater risk, such as:
- Seniors;
- Newborns;
- People with impaired immunity due to diseases such as AIDS, post-transplant or immunosuppressive drugs;
- Diabetes mellitus poorly controlled;
- People who are bedridden or have a change in consciousness, because they present a higher risk of aspiration;
- Vascular diseases, with impairment of the circulation, since it hinders the oxygenation and cicatrization of the tissues;
- Patients with need for invasive devices, such as urinary catheterization, venous catheter insertion, use of device ventilation;
- Performing surgeries.
In addition, the longer the hospitalization time, the greater the risk of acquiring a hospital infection, since there is a greater chance of exposure to the risks and to the responsible microorganisms.