Progressive ossifying fibrodysplasia, also known as FOP, progressive ossifying myositis or stone man syndrome, is a very rare genetic disease that causes the soft tissues of the body, such as ligaments, tendons, or muscles, to slowly turn into bone, hindering body movements and causing strong changes in body image.
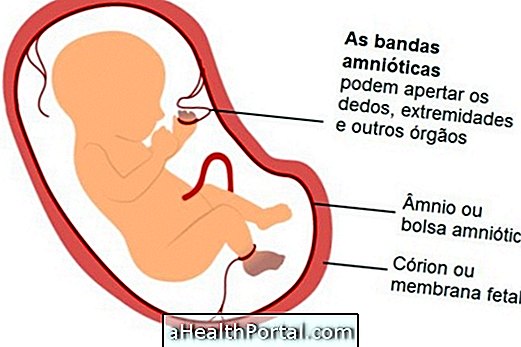
In most cases the symptoms appear during childhood, but the transformation of the tissues into bone continues into adulthood, and may vary the age at which the diagnosis is made. However, there are many cases where at birth the baby already has malformations of the toes or ribs that may lead the pediatrician to suspect the disease.
Although there is no cure for progressive ossifying fibrodysplasia, it is important that the child is always accompanied by the pediatrician, since there are forms of treatment that can help relieve some symptoms, such as swelling or joint pain, improving the quality of life.

Main symptoms
The first sign of progressive ossifying fibrodysplasia usually appears soon after birth with the presence of malformations of the toes and, in some cases, the thumbs.
The other symptoms usually appear until the age of 20 and include:
- Bumps reddened by the body, which disappear but leave bone in place;
- Bone development in puncture sites;
- Gradual difficulty to move hands, arms, legs or feet;
- Problems of blood circulation in the limbs.
In addition, depending on the affected regions, the development of cardiac or respiratory problems is also common, especially when frequent respiratory infections occur.
Progressive ossifying fibrodysplasia usually first affects the neck and shoulders, then progresses to the back, trunk, and limbs.
Although the disease can cause several limitations over time and dramatically decrease quality of life, life expectancy is usually long because there are usually no very serious life-threatening complications.
What causes and how the diagnosis is made
The specific cause of progressive ossifying fibrodysplasia and the process by which tissues become bone are still not well known, however, the disease arises due to a genetic mutation on chromosome 2. Although this mutation can be passed from parent to child, it is more common that the disease arises at random.
Since it is caused by a genetic change and there is no specific genetic test for it, the diagnosis is usually made by the pediatrician through the evaluation of symptoms and analysis of the child's medical history. This is because, other tests like the biopsy, cause small traumas that can lead to the development of bone in the examined place.
How is the treatment done?
There is no form of treatment capable of curing the disease or preventing its development, so it is very common for most patients to be confined to a wheelchair or bed after the age of 20.
When respiratory infections such as colds or flu come on, it is very important to go to the hospital soon after the first symptoms to start treatment and prevent serious complications in these organs. In addition, maintaining good oral hygiene also avoids the need for dental treatment, which can result in new bone formation crises, which can accelerate the rhythm of the disease.
Although limited, it is also essential to promote leisure and socialization activities for people with the disease, since their intellectual and communication skills remain intact and developing.