Collagen disease, also known as collagen disease, is characterized by a group of autoimmune and inflammatory diseases that damage the connective tissue of the body, which is the tissue formed by fibers, such as collagen, and is responsible for functions such as filling the spaces between organs, give sustenance, besides helping in the defense of the body.
The changes caused by collagenoses can reach various organs and systems of the body, such as skin, lungs, blood vessels and lymphatic tissues, for example, and produces mainly dermatological and rheumatologic signs and symptoms, which include joint pain, skin lesions, or dry mouth and eyes.
Some of the major diseases classified as collagenosis are:
1. Lupus

It is the major autoimmune disease, which causes lesions in organs and cells due to the action of autoantibodies, and is more common in young women, although it may appear in anyone. Its cause is still not completely understood, and this disease usually develops slowly and continuously, with symptoms that can be mild to severe, which varies from person to person.
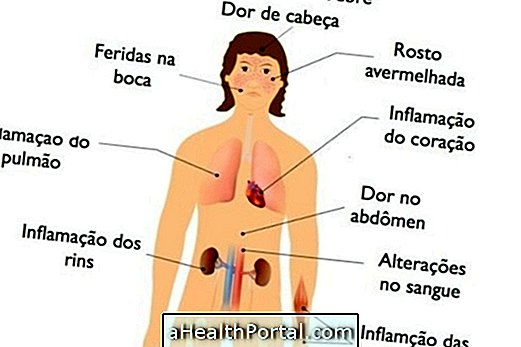
- Signs and symptoms : Lupus can cause a wide variety of clinical manifestations, ranging from localized to spread throughout the body, including skin blemishes, oral ulcers, arthritis, kidney changes, blood disorders, inflammation of the lungs and heart.
Learn more about what it is and how to identify lupus.
2. Scleroderma

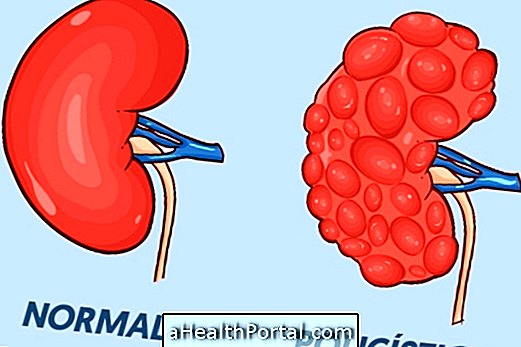
Also known as systemic sclerosis, it is a disease that causes accumulation of collagen fibers in the body, yet unknown cause, and mainly affects the skin and blood circulation in this organ, and can also reach internal organs such as lungs, heart, kidneys and gastrointestinal tract.
- Signs and symptoms : There is usually thickening of the skin, which becomes stiffer, shiny and with circulatory difficulties, which worsens slowly and continuously. When it reaches internal organs, in its diffuse type, it can cause respiratory difficulties, digestive alterations, besides compromising the functions of the heart and kidneys, for example.
Understand the symptoms of major types of scleroderma and how to treat it.
3. Sjögren's syndrome

It is another type of autoimmune disease characterized by the infiltration of defense cells into the body's glands, making it difficult to secrete the lacrimal and salivary glands. This disease is more common in middle-aged women, but it can occur in any person, and can arise in isolation or accompanied by diseases such as rheumatoid arthritis, lupus, scleroderma, vasculitis or hepatitis, for example.
- Signs and symptoms : Dry mouth and eyes are the main symptoms, which can worsen slowly and progressively, causing redness, burning and feeling of sand in the eyes or difficulty swallowing, speaking, increased tooth decay and a burning sensation in the mouth . Symptoms in other parts of the body are more rare, but may include fatigue, fever and joint and muscle pain, for example.
Understand better how to identify and diagnose Sjögren's syndrome.
4. Dermatomyositis

It is also a type of autoimmune disease that attacks and compromises muscles and skin. When it affects only the muscles, it can also be known as polymyositis. Its cause is unknown, and can occur in people of all ages.
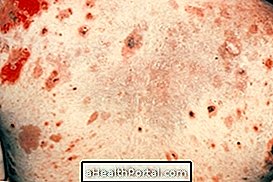
- Signs and symptoms : It is common to have muscle weakness, more common in the trunk, making movements of the arms and the basin difficult, such as combing the hair or sitting / lifting. However, any muscle can be affected, causing difficulty swallowing, moving the neck, walking or breathing, for example. Skin lesions include reddish or purplish spots and scaling that may worsen with the sun.
Learn more about how to identify and treat dermatomyositis.
How To Treat Collagenosis
The treatment of a collagenosis, as well as any autoimmune disease, depends on its type and severity, and should be directed by the rheumatologist or dermatologist. It usually involves the use of corticosteroids, such as Prednisone or Prednisolone, in addition to other immunosuppressants or more potent immunity regulators such as azathioprine, methotrexate, cyclosporin or Rituximab, for example, as a way to control immunity and decrease its effects on the body.
In addition, some measures like sun protection to prevent skin lesions, and artificial drops or saliva to decrease dry eyes and mouth, may be alternatives to lessen the symptoms.
Collagenosis has no cure, however, science has sought to develop more modern therapies based on the control of immunity with immunotherapy, so that these diseases can be controlled more effectively.
Main causes
There is still no clear cause for the emergence of the group of autoimmune diseases that cause collagenosis. Although they are related to the erroneous and excessive activation of the immune system, it is not known exactly what causes this situation.
Genetic and even environmental mechanisms such as lifestyle and eating habits are likely to be the cause of these diseases, however, science still needs to better determine these suspicions through further study.
To diagnose collagenosis, in addition to clinical evaluation, the physician may order blood tests that identify the inflammation and antibodies present in these diseases, such as FAN, Mi-2, SRP, Jo-1, Ro / SS-A or La / B, for example. Biopsies or tissue analysis with inflammation may also be required.