Diabetic neuropathy is one of the main complications of diabetes, characterized by progressive degeneration of the nerves, which can decrease the sensitivity or cause the appearance of pain in various parts of the body, being more common in the extremities such as the hands or feet.
Generally, diabetic neuropathy is more common in people who do not adequately treat diabetes, often with high blood sugar levels, which cause progressive nerve damage.
The development of peripheral neuropathy can be slow, with no symptoms in the early stages, but over time pain, tingling, burning sensation or loss of sensation in the affected region may appear.
Diabetic neuropathy has no cure, but its evolution can be controlled with the use of drugs to reduce blood sugar levels and to relieve neuropathic pain. Find out more about how neuropathic pain is treated.

Main symptoms
Diabetic neuropathy develops slowly and can go unnoticed until more severe symptoms appear. Symptoms vary according to the type of neuropathy:
1. Peripheral neuropathy
Peripheral neuropathy is characterized by the involvement of peripheral nerves, being the most common type of diabetic neuropathy. It usually starts at the feet and legs, followed by the hands and arms. Symptoms usually get worse at night and include:
- Numbness or tingling in the fingers or toes;
- Reduced ability to feel pain or changes in temperature;
- Burning sensation;
- Pain or cramps;
- Greater sensitivity to touch;
- Loss of touch;
- Muscle weakness;
- Loss of reflexes, especially in the Achilles' heel;
- Loss of balance;
- Loss of motor coordination;
- Deformity and joint pain.
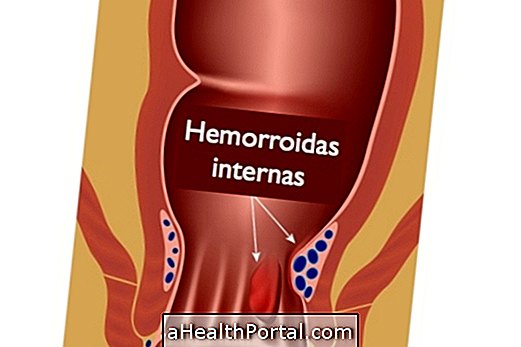
In addition, peripheral neuropathy can cause serious foot problems, such as the diabetic foot, characterized by ulcers or infections. Better understand what the diabetic foot is and how to treat it.
2. Autonomic neuropathy
Autonomic neuropathy affects the autonomic nervous system that controls various organs that function independently of the will, such as the heart, bladder, stomach, intestines, sexual organs and eyes.
The symptoms of neuropathy depend on the affected area and include:
- Absence of symptoms of hypoglycemia, such as confusion, dizziness, hunger, tremor or decreased motor coordination;
- Constipation or diarrhea;
- Nausea, vomiting, difficulty digesting or difficulty swallowing;
- Vaginal dryness;
- Erectile dysfunction;
- Increased or reduced sweat production;
- Decreased blood pressure that can cause dizziness when standing up;
- Feeling of a racing heart, even when standing still;
- Bladder problems such as needing to urinate frequently or having an urgent need to urinate, urinary incontinence or frequent urinary tract infection.
In addition, autonomic neuropathy can cause difficulty in visual adjustment of light in a dark environment.
3. Proximal neuropathy
Proximal neuropathy, also called diabetic amyotrophy or radiculopathy, is more common in the elderly and can affect the nerves in the thighs, hips, buttocks or legs, in addition to the abdomen and chest.
Symptoms usually occur on one side of the body, but they can spread to the other side and include:
- Severe pain in the hip and thigh or buttocks;
- Stomachache;
- Weakness in the thigh muscles;
- Difficulty getting up from a sitting position;
- Abdominal swelling;
- Weight loss.
People with proximal neuropathy may also have a dropped or flabby foot, as if the foot is relaxed, which can cause difficulty walking or falls.
4. Focal neuropathy
Focal neuropathy, also called mononeuropathy, is characterized by the involvement of a specific nerve in the hands, feet, legs, trunk or head.
Symptoms depend on the affected nerve and include:
- Loss of sensation in the area of the affected nerve;
- Tingling or numbness in the hands or fingers due to compression of the ulnar nerve;
- Weakness in the affected hand, which can make it difficult to hold objects;
- Pain in the outside of the leg or weakness in the big toe, due to compression of the peroneal nerve;
- Paralysis on one side of the face, called Bell's palsy;
- Vision problems such as difficulty in focusing on an object or double vision;
- Pain behind the eye;
In addition, other symptoms, such as pain, numbness, tingling or burning sensation in the thumb, index finger and middle finger, may occur due to compression of the median nerve, which passes through the wrist and unnerves the hands, characterizing the carpal tunnel syndrome. Learn more about Carpal Tunnel Syndrome.
How to confirm the diagnosis
The diagnosis of diabetic neuropathy is made by the endocrinologist and is based on the signs and symptoms presented and the history of the disease. In addition, the doctor must perform a physical exam to check the strength and muscle tone, test the tendon reflex and analyze the sensitivity to touch and changes in temperature, such as cold and heat.
The doctor can also perform or order specific tests to confirm the diagnosis, such as a nerve conduction test, which measures how quickly the nerves in the arms and legs conduct electrical signals, electroneuromyography, which measures the electrical discharges produced in the muscles, or autonomic test, which can be done to determine changes in blood pressure at different positions.
How the treatment is done
Treatment for diabetic neuropathy should be guided by an endocrinologist and is usually done to relieve symptoms, avoid complications and slow the progression of the disease.
Treatments for diabetic neuropathy include medications such as:
- Antidiabetics, such as insulin injections or taking oral antidiabetics, to control blood sugar levels;
- Anticonvulsants, such as pregabalin or gabapentin to relieve pain;
- Antidepressants, such as amitriptyline, imipramine, duloxetine or venlafaxine that help relieve mild to moderate pain;
- Opioid analgesics taken orally, such as tramadol, morphine, oxycodone or methadone, or patch, such as transdermal fentanyl or transdermal buprenorphine.
In some cases, the antidepressant can be used in conjunction with an anticonvulsant or these medications can be used with pain relievers to help control pain.
In addition, for the treatment of complications of diabetic neuropathy, care may be necessary with different specialists, such as a urologist to treat urinary tract problems, with medications that regulate bladder function or remedies for erectile dysfunction, for example, or a cardiologist for control blood pressure and avoid diabetic cardiomyopathy. Find out what diabetic cardiomyopathy is and how to treat it.
How to prevent neuropathy
Diabetic neuropathy can usually be prevented if blood glucose levels are strictly controlled. To do this, some measures include:
- Regular medical follow-up;
- Monitor blood glucose levels at home with glucometers, according to medical advice;
- Take the medication or inject the insulin, as prescribed by the doctor;
- Practice physical activities on a regular basis such as light walking, swimming or water aerobics, for example.
You should also eat a balanced diet that includes good fibers, proteins and fats, and avoid foods with a lot of sugar like cookies, soft drinks or cakes. Check out how to diet for diabetes.
Was this information helpful?
Yes No
Your opinion is important! Write here how we can improve our text:
Any questions? Click here to be answered.
Email in which you want to receive a reply:
Check the confirmation email we sent you.
Your name:
Reason for visit:
--- Choose your reason --- DiseaseLive betterHelp another personGain knowledge
Are you a health professional?
NoMedicalPharmaceuticalsNurseNutritionistBiomedicalPhysiotherapistBeauticianOther
Bibliography
- BOULTON, Andrew J. M. Diabetic neuropathy and foot complications. Handbook of Clinical Neurology. 126. 97-107, 2014
- VINIK, Aaron I .; et al. Diabetic Neuropathy. Endocrinology and Metabolism Clinics of North America. 42. 747–787, 2013
- BERNAL, D. Samper; et al. Etiology and management of painful diabetic neuropathy. Revista de la Sociedad Española del Dolor. 17. 6; 286-296, 2010
- FELDMAN, Eva L .; et al. Diabetic neuropathy. Nat Rev Dis Primers. 2019 Jun 13; 5: 42 .. 5. 1; 1-40, 2019