Neonatal jaundice occurs when the skin, eyes, and mucous membranes of the body become yellowish due to excess bilirubin in the blood.
The main cause of jaundice in the baby is the physiological jaundice, which arises due to the liver's inability to metabolize and eliminate bilirubin, as it is still underdeveloped. It is usually not a cause for concern, and the treatment is done with phototherapy.
Bilirubin is a yellow pigment that is produced by the breakdown of blood cells in the body and is then taken up by the liver where it is bound to proteins and eliminated along with bile by the intestine, so changes in any of these phases may cause elevation of this pigment in the blood. Learn more about bilirubin in bilirubin test and its values.

What causes neonatal jaundice
Jaundice of the newborn or neonatal is a frequent problem, and the most common causes include:
- Physiological jaundice : it is the most common cause, which arises after 24 to 36 hours of birth, because the baby's liver is poorly developed and may present difficulties in transforming and eliminating bilirubin;
- Increased destruction of blood cells : this is a serious cause of jaundice due to blood diseases such as sickle cell anemia, spherocytosis, or hemolytic anemia, which may be caused by the incompatibility of the baby's blood with that of the mother. Learn more about this condition in: Fetal erythroblastosis;
- Breast milk jaundice : it occurs in infants who are exclusively breastfed, usually after about 10 days of birth, due to the increase of hormones or substances in the blood that increase the reabsorption of bilirubin in the intestine and make it difficult to eliminate it, although its causes are not yet entirely clear;
- Liver diseases : they are usually hereditary diseases, such as Crigler-Najjar syndrome, Gilber syndrome and Gaucher disease, for example;
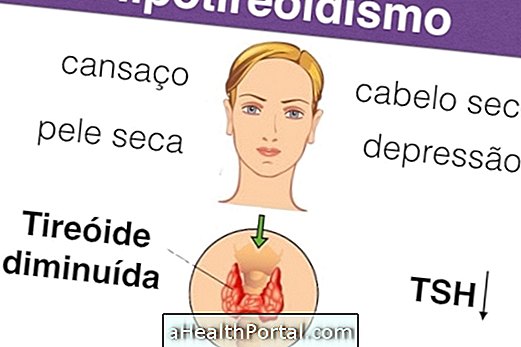
- Congenital diseases : which can be provoked during pregnancy, such as rubella or congenital hypothyroidism;
- Deformities in the biliary tract ;
- Infections with viruses or bacteria .
Understand the possible causes in: What causes and how to treat neonatal hyperbilirubinemia.
How to Identify Jaundice
Jaundice usually arises on the second day of life of the baby but in premature babies it tends to appear on the 5th day of life.
The yellowish color of the skin advances from the head towards the feet, being observed first in the face, later in the trunk and later in the feet. Gently pressing the baby's chest is a good way to identify jaundice outside the hospital. If the pressured region becomes yellowish, contact your doctor to begin treatment.
How to treat neonatal jaundice
Although jaundice is not always a serious condition or has serious consequences, proper treatment is necessary because, under rare circumstances, it can cause brain damage. This condition is called kernicterus and treatment in these cases involves a blood transfusion. Understand what is and what to do in case of kernicterus.
Phototherapy treatment
The phototherapy is done with the placement of the baby in a small crib where it is completely naked, using only diaper, being exposed to a special light, a treatment called phototherapy. While the baby is exposed to this fluorescent light, it must remain blindfolded with a protective mask.
In milder cases the pediatrician may recommend that the baby be exposed to the sun daily in the morning when the sun is still weak, always before 10 and after 16 hours. The treatment can last for 2 days and the exposure time to light can vary from 15 to 30 minutes at a time.
Understand more about how phototherapy works in which diseases phototherapy can treat.
Other forms of treatment
Breastfeeding the baby is a great way to complement the treatment, normalizing the baby's color faster as it reduces the reabsorption of bilirubin in the gut. In rare cases of "breast milk jaundice" breastfeeding may need to be discontinued for 1 or 2 days until the bilirubin concentration in the blood normalizes.
In the more severe cases of jaundice, such as infectious, congenital or genetic causes, the treatment is specific according to the cause, guided by the pediatrician, during hospitalization, and may involve antibiotics, corticoids, hormone therapy or, in the cases of very high bilirubin, the blood transfusion, which helps to remove bilirubin more quickly from the blood.