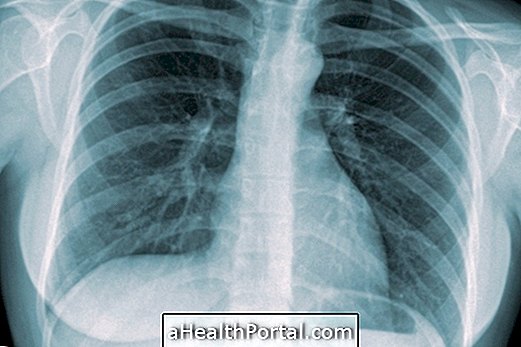
Pulmonary fibrosis is a disease characterized by the appearance of fibrosis, that is, scars on the tissue of the lungs, causing them to become more rigid, hampering respiratory capacity and causing symptoms such as shortness of breath and dry cough, for example.
In many cases the cause of the disease is not found, being classified as Idiopathic Pulmonary Fibrosis, but some factors that increase the chances of developing the disease are exposure to occupational dust, such as silica and asbestos, smoking, pollution, autoimmune diseases or side effect of use of certain medications, such as Amiodarone or Nitrofurantoin, for example.
Pulmonary fibrosis has no cure because these lung damage can not be repaired. However, the disease can be controlled through treatment involving physical therapy and the use of medications prescribed by the pulmonologist such as immunosuppressants, Pirfenidone or Nintedanibe. See how this medication works and how to use it by clicking here.

Main symptoms
At an early stage, pulmonary fibrosis may not cause symptoms. As the disease progresses, signs and symptoms such as:
- Shortness of breath;
- Dry cough or low secretion;
- Excessive tiredness;
- Lack of appetite and weight loss with no apparent cause;
- Muscle and joint pain;
- Blue or purple fingers;
- Deformity in the fingers characteristic of the lack of oxygenation of the organism, called "fingers in drumstick".
The severity and speed of onset of symptoms can vary from person to person, especially according to the cause, and usually evolves over months to years.
When pulmonary fibrosis is suspected, the pulmonologist will request tests such as computed tomography, which evaluates the presence of changes in lung tissue, spirometry, which measures lung ventilation capacity and other tests, such as blood tests, that pneumonia. In case of doubt, a pulmonary biopsy may be performed.
It is important not to confuse pulmonary fibrosis with cystic fibrosis, which is a hereditary disease that occurs in children, in which some glands produce abnormal secretions that primarily affect the digestive and respiratory tract. See how to identify and treat cystic fibrosis.
How is the treatment done?
Treatment of pulmonary fibrosis should be guided by a pulmonologist and usually includes medicines with antifibrotic properties such as Pirfenidone or Nintedanib, corticosteroids such as Prednisone, and medicines that reduce the immune system response, such as Ciclosporin or Methotrexate. alleviate some symptoms or delay the progression of the disease. .
Physiotherapy is fundamental to perform pulmonary rehabilitation, in which programmed exercises are done with the aim of improving the patient's respiratory capacity, which is more active and less symptomatic.
In addition, in more severe cases, the doctor may also recommend using oxygen at home as a way to help increase blood oxygenation. The disease can become very serious for some people, and in those cases, a lung transplant may be indicated.
Learn more about treatment in: Treatment for pulmonary fibrosis.
What causes pulmonary fibrosis
Although no specific cause is determined for pulmonary fibrosis, the risk of developing the disease is greater for individuals who:
- They are smokers;
- They work in environments with many toxins, such as silica or asbestos dust, for example;
- They do radiation therapy or chemotherapy for cancer, such as lung or breast cancer;
- They use certain drugs that may cause this effect, such as Amiodarone Hydrochloride or Propranolol, or antibiotics, such as Sulfasalazine or Nitrofurantoin, for example;
- They have lung diseases, such as Tuberculosis or Pneumonia;
- They have autoimmune diseases, such as lupus, rheumatoid arthritis or scleroderma.
In addition, idiopathic pulmonary fibrosis can be passed from parents to offspring, and genetic counseling is recommended if there are many cases of the disease in the family.