Rheumatic fever, popularly called rheumatism in the blood, is a disease caused by an autoimmune reaction of the body after infections caused by bacteria.
This disease is most common in children between the ages of 5 and 15 and usually generates symptoms such as pain and inflammation in the joints, as well as fever and tiredness. In addition, rheumatism in the blood can still affect the nervous system and even the heart valves, impairing the functioning of the heart.
Blood rheumatism should be treated as soon as the first symptoms appear, to prevent permanent damage to the brain or heart, which can lead to complications such as heart valve stenosis or heart failure, for example.

Main symptoms
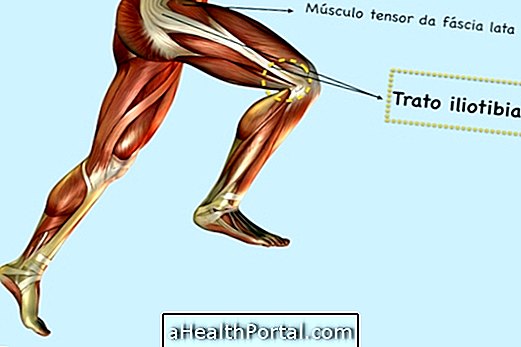
One of the first symptoms of rheumatism in the blood is the presence of inflammation in a joint that lasts 2 or 3 days, heals itself and then arises in another joint and so on.
However, it can also be accompanied by other symptoms such as:
- Fever above 38º C;
- Small nodules under the skin;
- Chest pain;
- Red spots on the skin.
Depending on whether or not cardiac involvement already exists, there may still be tiredness and increased heart rate. If there is a cerebral compromise, there may be behavioral changes, such as crying and tantrums, and motor changes, such as involuntary movements or convulsions.
See more signs of rheumatic fever.
Possible causes
The most common cause of rheumatism in the blood is a throat infection caused by the bacteria Streptococcus pyogenes, which is a beta-hemolytic group A streptococcus that was not readily treated.
The initial picture is a throat infection in which the body creates antibodies to fight the bacteria but later, and it is unclear why, these antibodies end up fighting the bacteria and healthy joints of the body.
Individuals with the HLA-B27 gene, which is the gene for rheumatism, are highly likely to develop rheumatic diseases such as spondyloarthritis, Reiter's syndrome or ankylosing spondylitis, for example.
The rheumatism gene may be present in 8% of the world's population and is identified in a simple blood test called the genetic test.
Although the presence of the rheumatism gene indicates that the individual will most likely develop rheumatic diseases, they should only be diagnosed in adulthood after the onset of the characteristic symptoms of each disease, and it may be that the individual reaches the end of life without presenting any rheumatic disease.
How to confirm the diagnosis
There is no single test that allows the diagnosis of rheumatism in the blood, so the doctor can not only evaluate the symptoms, but can also order various tests such as electrocardiogram, echocardiogram and blood test, such as the ASLO exam. Find out what it is for and how the ASLO exam is done.
How is the treatment done?
The primary goal of treatment is to eliminate the bacteria that caused the initial infection to relieve symptoms and reduce inflammation in the body. For this, several drugs can be prescribed:
- Antibiotics, such as Penicillin: help eliminate the remaining bacteria;
- Anti-inflammatories, such as Naproxen or Diclofenac: relieve inflammation and joint pain and may also relieve fever;
- Anticonvulsants, such as Carbamazepine or Valproic Acid: decrease the onset of involuntary movements.
- Corticosteroids, like Cortisone: improve cardiac involvement.
In addition, it is important to maintain rest if the pain in the joints is very intense and drink plenty of water to aid in the functioning of the immune system. Understand better how the treatment is done.