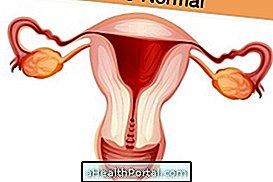
The endometrium is the tissue that internally coats the uterus and its thickness varies throughout the menstrual cycle according to the variation of the concentration of hormones in the bloodstream.
It is in the endometrium that the implantation of the embryo occurs, initiating the pregnancy, but for that to happen, the endometrium must have the ideal thickness and have no sign of disease. When there is no fertilization, tissue desquamation occurs, menstruation being characterized.

Endometrial changes in phases
The thickness of the endometrium varies every month in all women of reproductive age, characterizing the phases of the menstrual cycle:
- Proliferative phase: Soon after menstruation the endometrium is completely desquamated and ready to increase in size, this phase is called proliferative, and in this period estrogen promotes the release of cells that increase its thickness, as well as blood vessels and exocrine glands.
- Secretory Phase: In the secretory phase, which occurs during the fertile period, estrogen and progesterone will cause the endometrium to have all the nutrients needed for the implantation and nutrition of the embryo. If there is fertilization and the embryo can stay in the endometrium, a rosy 'discharge' or coffee grounds may be observed during its fertile day, but if there is no fertilization, after a few days the woman will menstruate. Learn to recognize the symptoms of fertilization and nesting.
- Menstrual phase: If fertility does not occur during the fertile period, which is when the endometrium is thicker, this tissue will now enter its menstrual phase and will decrease in thickness due to sudden drop of hormones in the bloodstream and decrease of irrigation of the fabric. These changes cause the endometrium to release gradually from the uterine wall, giving rise to the bleeding that we know from menstruation.
The endometrium can be evaluated by gynecological imaging, such as pelvic ultrasonography, colposcopy, and MRI, for example, where the gynecologist checks for signs of disease or changes in the tissue. Get to know other exams requested by the gynecologist.
Endometrium in pregnancy
The ideal endometrium to conceive is the one that measures about 8 mm and is in the secretory phase, because the thin or atrophic endometrium, measuring less than 6 mm, is not able to allow the baby to develop. The main cause of fine endometrics is the lack of progesterone, but this can also happen due to contraceptive use, infant uterus and lesions after abortion or curettage.
The minimum pregnancy thickness is 8 mm and the ideal thickness is approximately 18 mm. In women where this does not occur naturally the doctor may prescribe the use of hormonal drugs such as Utrogestan, Evocanil or Duphaston to increase the endometrial thickness, facilitating the implantation of the embryo in the uterus.
The reference thickness of the endometrium after menopause is 5 mm, which can be observed on transvaginal ultrasonography. At this stage, when the thickness is greater than 5 mm the doctor will ask for a series of other tests to better evaluate the woman and be alert to other signs that may reveal possible diseases such as endometrial cancer, polyp, hyperplasia or adenomyosis, for example .

Major diseases affecting the endometrium
The alterations of the endometrium may be due to diseases that can be treated and controlled with the use of hormones and, in some cases, surgery. Medical monitoring is essential to avoid complications of each disease, maintain uterine health and increase the chances of becoming pregnant. The most common diseases related to the endometrium are:
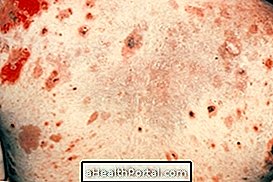
1. Endometrial cancer
The most common disease that affects the endometrium is endometrial cancer. This can be easily discovered because its main symptom is bleeding out of menstruation. In the case of women who have already passed the menopause and have not menstruated for 1 year, the symptom is soon perceived.
For those who have not yet reached menopause the main symptom is the increased amount of blood lost during menstruation. You have to be attentive to these signs and look for a gynecologist soon, because the sooner the problem is discovered, the greater the chances of a cure. Learn how to identify endometrial cancer.
Endometrial polyp
Polyps located in the region of the endometrium are benign and easily noticed because it generates symptoms such as blood loss before or after menstruation or difficulty getting pregnant. This change is most common after menopause and usually occurs in women taking medications such as Tamoxifen.
Most of the time this disease is discovered on an ultrasound that shows an increase in its thickness. The treatment is the gynecologist's choice but can be done with polyp withdrawal through surgery, especially if the woman is young and wants to become pregnant, but in many cases it is not necessary to perform surgery, nor to take hormonal medications, case every 6 months to check for any changes.
3. Endometrial hyperplasia
Increased endometrial thickness is called endometrial hyperplasia, being more common after 40 years of age. Its main symptom is bleeding outside the menstrual period, in addition to pain, abdominal colic and enlargement of the uterus, which can be seen on a transvaginal ultrasonography.
There are several types of endometrial hyperplasia and not all are cancer related. Your treatment may involve hormonal medications, curettage, or surgery in the most severe cases. Learn more about endometrial hyperplasia ..
4. Adenomyosis
Adenomyosis occurs when the tissue inside the uterine walls increases in size causing symptoms such as heavy bleeding during menstruation and cramps that hinder the woman's life, as well as pain during intimate contact, constipation and abdominal bloating. Its causes are not fully known, but can happen due to gynecological surgeries or cesarean delivery, for example, in addition adenomyosis may arise after pregnancy.
The treatment can be done with the use of contraceptives, IUD placement or surgery to remove the uterus, in the most severe cases, when the symptoms are very uncomfortable and when there is contraindication to the use of hormonal drugs. Learn more about Adenomyosis.