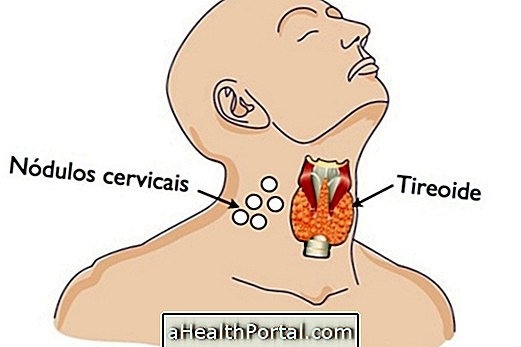
Hyperthyroidism may occur before or during pregnancy, and when left untreated may cause problems such as preterm birth, hypertension, placental abruption, and miscarriage.
This disease can be detected through a blood test, and its treatment is done with the use of drugs that regulate thyroid function. After delivery, it is necessary to continue the medical follow-up, since it is common for the disease to remain throughout the woman's life.
Complications for mother and baby
When untreated, hyperthyroidism can lead to complications for both mother and baby, such as:
- Premature birth;
- Low weight at birth;
- Hypertension in the mother;
- Thyroid problems for the baby;
- Displacement of the placenta;
- Heart failure in the mother;
- Abortion;
It is important to remember that in most cases women already had symptoms of the disease before pregnancy and so do not realize the changes caused in the body when they become pregnant. The most common thyroid disease during pregnancy is Strikes Disease, so look at its symptoms and treatment here.

Symptoms
The symptoms of hyperthyroidism in pregnancy are often confused with the natural symptoms that occur in the woman's body due to hormonal changes such as:
- Excessive heat and sweat;
- Tiredness;
- Anxiety;
- Accelerated heart;
- Nausea and vomiting of great intensity;
- Weight loss or inability to gain weight, even if feeding well.
So the main sign that something may be wrong with the thyroid is the absence of weight gain, even with increased appetite and the amount of food consumed.
How to diagnose
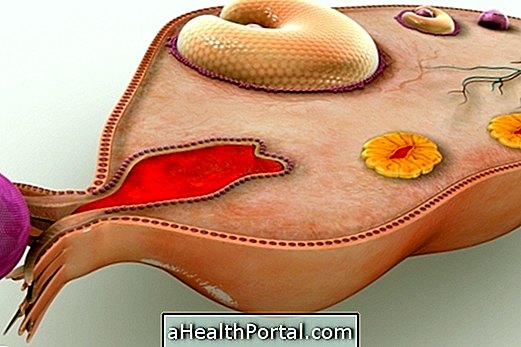
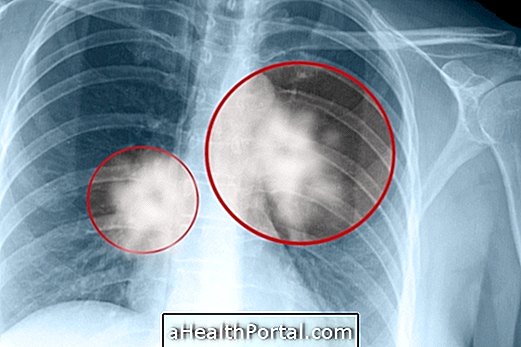
The diagnosis of hyperthyroidism in pregnancy is done through blood tests that evaluate the amount of hormones T3, T4 and TSH in the body. When these hormones are elevated, it can be a sign of thyroid disease.
However, it is important to remember that the T4 hormone may be elevated due to high levels of beta-HCG in the blood, especially between the 8th and the 14th week of gestation, returning to normal after this period.
How to treat
The treatment of hyperthyroidism in pregnancy is done with the use of drugs that regulate the production of thyroid hormones, such as Tapazole or Propylthiouracil.
Initially, larger doses are given to control hormones more quickly, and after 6 to 8 weeks of treatment, if the woman improves, the dose of the drug is reduced and may even be discontinued after 32 or 34 weeks of gestation.
Postpartum Care
After delivery, it is necessary to continue taking thyroid medicines, but if the medication is discontinued, new blood tests should be done to evaluate the hormones 6 weeks after delivery, as it is common for the problem to recur.
In addition, during the breastfeeding period it is recommended that medications be taken at the lowest possible doses, preferably soon after the baby's feeding.
It is also important to remember that children should have routine tests to evaluate thyroid function as they are more likely to have hyper or hypothyroidism.
After the baby is born, see how to treat hyperthyroidism.
See feeding tips to treat and prevent thyroid problems by watching the following video: