Symptoms of malaria may occur 1 to 4 weeks after infection with Plasmodium protozoa , and include severe headache, malaise, chills with tremors, and fever arising in a cyclic pattern that appears every 2 to 3 days, and relieves after 6 to 12 hours.
This infection is transmitted through the female bite of the Anopheles type mosquito, which in Brazil is more common in the Amazon region, although it may occur in any of the other states.
Although it is usually mild to moderate, malaria can develop severe conditions, so diagnosis should be made as early as possible, since correct and rapid treatment are the most appropriate ways to reduce the severity and mortality of this disease.

First symptoms
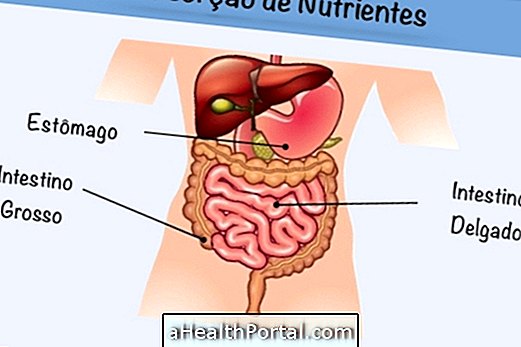
The first symptoms of malaria appear after about 8 to 30 days after the bite, which varies according to the species of Plasmodium and the amount transmitted, in addition to the defense system of the infected person. In this period, the microorganisms are reproducing inside the cells of the liver, causing no symptoms.
Then the parasites reach the cells of the bloodstream, causing symptoms such as:
- Fever, which can reach 40ºC;
- Tremors and chills;
- Intense sweating;
- Pains throughout the body;
- Headache;
- Weakness;
- General malaise;
- Nausea and vomiting.
It is common for fever and the intensification of symptoms to occur suddenly every 2 to 3 days for about 6 to 12 hours, when the red blood cells rupture and the parasites circulate in the bloodstream, a very characteristic malaria situation .
However, disease patterns vary depending on the type of malaria, whether it is complicated or not, and the complications can be fatal.
Signs and symptoms of cerebral malaria
In some cases, the infection can develop serious complications, and cerebral malaria is the most common and important. Some symptoms that indicate cerebral malaria include:
- Stiff neck;
- Disorientation;
- Somnolence;
- Convulsions;
- Vomiting |
- Coma state.
Cerebral malaria can be life threatening and is commonly mistaken for other serious neurological diseases such as meningitis, tetanus, epilepsy, and other neurological disorders.
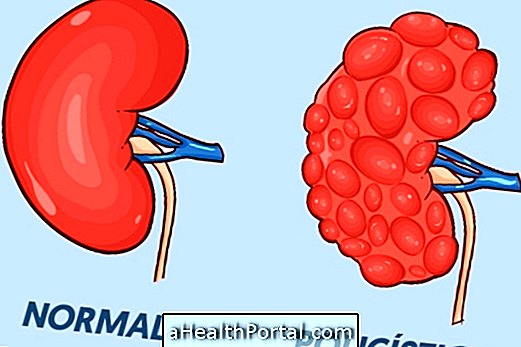
Other complications of malaria include anemia, reduced platelets, kidney failure, jaundice and respiratory failure, which are also severe, and should be monitored throughout the course of the disease.
How to know if it is malaria
The diagnosis of malaria is made by microscopic examination of the blood test, also known as thick blood smear, requested by the doctor. This test should be available at the health post or hospital, especially in areas most affected by malaria, and it is done whenever symptoms that indicate the infection appear.
In addition, new immunological tests have been developed to facilitate and expedite the confirmation of malaria. If the result indicates malaria really, the doctor may also ask for other tests to monitor and evaluate possible complications, such as a blood count, urine test and chest x-ray, for example.
How to treat malaria
The goal of malaria treatment is to destroy Plasmidium and request its transmission with antimalarial drugs. there are different treatment regimens, which varies according to the Plasmodium species, age of the patient, severity of the disease and whether there are other associated health conditions such as pregnancy or other diseases.
The remedies used may be Chloroquine, Primaquine, Artemeter and Lumefantrine or Artesunate and Mefloquine, for example. Children, infants, and pregnant women can be treated with Quinine or Clindamycin, always in accordance with medical recommendations, and hospitalization is usually indicated as this is a serious and potentially fatal disease.
People who live in places where this disease is frequent can get malaria more than once, babies and children are easily bitten by mosquitoes and so can develop this disease several times during life. It is important to remember that treatment should be started as soon as possible because there may be complications that can lead to death. Learn more details on how treatment is done and how to recover faster.