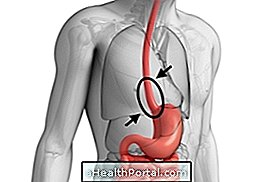
Boerhaave syndrome is a rare problem that consists of the spontaneous onset of a ruptured esophagus that causes symptoms such as severe chest pain and a feeling of shortness of breath, for example.
Generally, Boerhaave's syndrome is caused by excessive intake of food or alcohol that causes intense vomiting, increasing abdominal pressure and overexercising the esophageal muscles that eventually tear.
Boerhaave syndrome is a medical emergency so it is important to go to the hospital immediately if there is acute chest pain or shortness of breath to start treatment within the first 12 hours and avoid serious complications such as respiratory arrest.

Symptoms of Boerhaave's syndrome
The main symptoms of Boerhaave syndrome include:
- Severe chest pain that worsens on swallowing;
- Feeling of shortness of breath;
- Swelling of the face or throat;
- Changing the voice.
Usually, these symptoms appear after vomiting, but in some cases may also appear some time later when eating or drinking water, for example.
In addition, the symptoms vary in each case, and may present other completely different signs like excessive desire to drink water, fever or constant vomiting. In this way, the diagnosis is usually time-consuming because the syndrome can be confused with other cardiac or gastrointestinal problems.
Treatment for Boerhaave's syndrome
Treatment for Boerhaave syndrome should be done at the hospital with emergency surgery to correct rupture of the esophagus and treat the infection that usually develops in the chest due to accumulation of gastric acids and bacteria from food.
Ideally, treatment should be initiated within the first 12 hours after esophageal rupture to prevent the development of a general infection that, after that time, halves the life expectancy of the patient.
Diagnosis of Boerhaave's syndrome
The diagnosis of Boerhaave syndrome can be made by chest X-ray and computed tomography, however, it is important to have access to the patient's history to exclude other diseases with similar symptoms, such as gastric ulcer perforation, acute myocardial infarction or acute pancreatitis, which are more common and may cover up the syndrome.
Thus, it is recommended that the patient should always be followed, whenever possible, by a relative or close person who knows the clinical history of the patient or who can describe the time of onset of symptoms, for example.