Treatment for pancreatic cancer varies according to organ involvement, the degree of cancer development, and the onset of metastases, for example.
Thus, each case should be evaluated by an oncologist in order to choose one of the following forms of treatment:
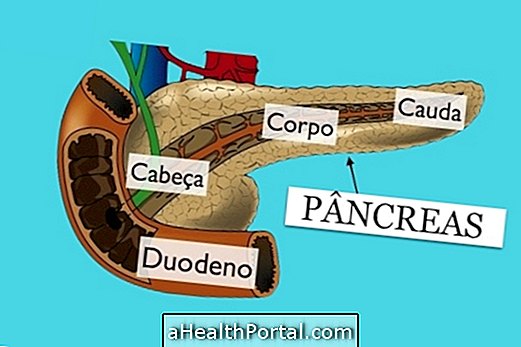
- Surgery : It is usually done when the cancer has not yet developed out of the organ. In surgery the affected region of the pancreas is removed, as well as other organs that are at great risk of being affected, such as intestine or gallbladder;
- Radiation therapy : may be used before surgery to decrease the size of the tumor, or after surgery to eliminate the remaining cancerous cells;
- Chemotherapy : It is usually used in more advanced cases and uses medicines directly into the vein to destroy cancer cells. When metastases are present, this treatment can be combined with radiotherapy for best results.
In addition, there are still alternative forms of treatment that can not guarantee the cure of the disease, but may help relieve some symptoms or even improve the effect of medical treatment.

Although there are several ways to cure pancreatic cancer, treatment is usually very difficult because as this disease does not cause symptoms in the early stages, it is usually only identified when the cancer has already spread to other organs.
If the treatment fails to combat cancer, the oncologist usually advises palliative treatment, which helps relieve symptoms and improve comfort during the last few days of the person.
Chemotherapy for pancreatic cancer
Chemotherapy is one of the most commonly used treatment options for pancreatic cancer, especially in cases of exocrine cancer, which is the most common and most serious type.
Generally, chemotherapy can be used in 3 different ways during treatment:
- Before surgery : it helps to reduce the size of the tumor, facilitating its removal during surgery;
- After the surgery : it allows to eliminate the cancerous cells that were not removed with the surgery;
- Instead of surgery : when the surgery can not be used because the cancer is already widespread or the person does not have the conditions to be operated on.
In addition, chemotherapy may still be associated with radiation therapy, which uses radiation to kill cancer cells, having a more potent action when used together.
In most cases, chemotherapy is done by cycles, and it is common to do 1 to 2 weeks of treatment, interspersed with a rest period for the body to recover.
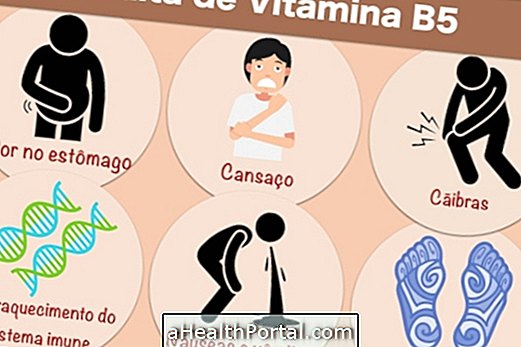
The side effects of chemotherapy in the body vary depending on the medicine used and its dosage, however, the most common include vomiting, nausea, loss of appetite, hair loss, mouth sores, diarrhea, constipation, excessive tiredness and bleeding. In addition, people undergoing chemotherapy also have a higher risk of developing infections. Learn more about the side effects of chemotherapy in the body and how to deal with them.
Usually used remedies
Some of the medicines most used in the chemotherapy treatment of pancreatic cancer are:
- Gemencitabine;
- Erlotinib;
- Fluorouracil;
- Irinotecan;
- Oxaliplatin;
- Capecitabine;
- Paclitaxel;
- Docetaxel.
These medicines can be used separately or in combination, depending on the state of health of each patient.
In cases of end-stage pancreatic cancer, the use of these drugs is not necessary, and it is recommended only to take strong analgesics to reduce the patient's pain at the end of life.
Causes of Pancreatic Cancer
Some of the causes of pancreatic cancer are:
- Smoking actively or passively
- Excessive consumption of fats, meat and alcoholic beverages
- Exposure to chemicals such as petroleum derivatives and paint solvents, for example
- In case of chronic pancreatitis or diabetes mellitus that is not properly treated
All of the above causes are related to an overload in the pancreas and any other disease that may in some way affect the compromise of this organ can also end up generating pancreatic cancer.
Individuals who have severe digestive problems such as chronic pancreatitis or who have undergone surgery to repair an ulcer in the stomach, duodenum or who have undergone gallbladder removal are more likely to develop pancreatic cancer and should be alert to first signs and symptoms of the disease.
Performing blood tests, stool, urine every 6 months may be helpful and if any of these tests show significant changes, your doctor may prescribe CT or MRI scans to look at the internal organs. If the doctor thinks that the pancreas or the liver is compromised, biopsy of the tissue may show the presence of cancer cells.

How palliative treatment is done
Palliative treatment of pancreatic cancer is indicated when the disease is discovered at a very advanced stage and the chances of cure with medical treatment are minimal. This type of treatment is intended to decrease the pain and discomfort of the patient, and can be done in hospital or home stay with the use of strong analgesics that can relieve the pain.
If discovered at an advanced stage, understand the life span of a person with pancreatic cancer.
How to live with pancreatic cancer
Living with pancreatic cancer is not easy for the patient or the family. The patient should start the treatment by staying in an oncology hospital as soon as the disease is diagnosed to initiate treatment.
Initiating treatment promptly is important because the later the treatment is started, the more the disease spreads and the shorter its life span and fewer treatment alternatives will be possible.
Life span of individuals with pancreatic cancer
The survival rate of the pancreatic cancer patient varies from 6 months to 5 years and will depend on the size, location and whether the tumor has metastasized or not.
After medical observation and appropriate clinical studies, the patient may be sent home, but should return on the days determined by the doctors to do the surgery to remove the tumor to continue the drug treatment and if necessary, to perform the radiotherapy sessions.
Rights of patients with pancreatic cancer
To ensure patient and family, the cancer patient has some rights such as:
- Withdrawal from FGTS, PIS / PASEP;
- Free public transport;
- Priority in the progress of legal proceedings;
- Disease aid;
- By disability retirement;
- Exemption from Income Tax;
- Benefit of the benefit guaranteed by INSS (receive 1 minimum monthly salary);
- Free medications;
- Receive the private pension plan.
Other entitlements include receiving an indemnity due to life insurance and home discharge, depending on the contract signed by the patient before being diagnosed with the illness.