Dysmenorrhoea is characterized by a very severe colic during menstruation, which prevents even the woman from studying and working, from 1 to 3 days, every month. It is more common in adolescence, although it can affect women over 40 or girls who have not started menstruating.
Although it is very intense, and can cause disruption to a woman's life, this colic can be controlled with medicines such as anti-inflammatories, analgesics and the birth control pill. Therefore, in case of suspicion you should go to the gynecologist to investigate if it really is dysmenorrhea, and which remedies are most indicated.

Differences between primary and secondary dysmenorrhea
There are two types of dysmenorrhea, the primary and the secondary, and the differences between them are related to the origin of the colic:
- Primary dysmenorrhea: prostaglandins, which are substances produced by the uterus itself, are responsible for the intense menstrual colic. In this case the pain exists without any type of disease involved, and begins 6 to 12 months after the first menstruation, can cease or reduce by the age of 20, but in some cases only after pregnancy.
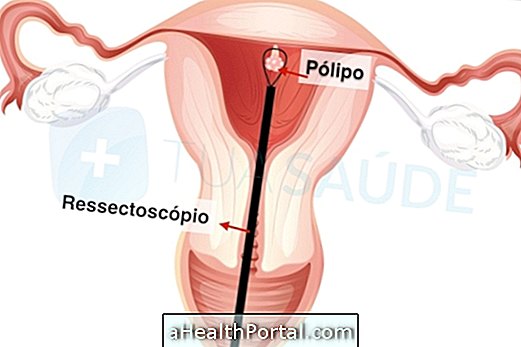
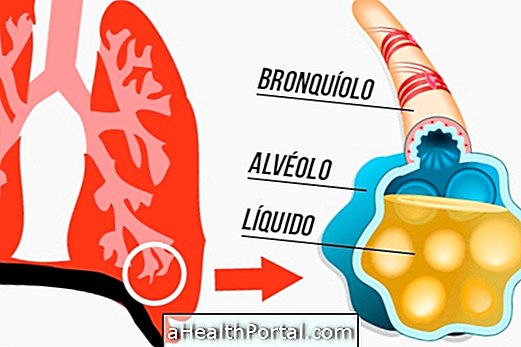
- Secondary dysmenorrhea: it is related to diseases such as endometriosis, which is the main cause, or in case of myoma, ovarian cyst, IUD use, pelvic inflammatory disease or abnormalities in the uterus or vagina, which the doctor finds when performing tests.
Knowing if the woman has primary or secondary dysmenorrhea is essential to start the treatment most appropriate for each case. The following table shows the main differences:
| Primary dysmenorrhoea | Secondary dysmenorrhoea |
| Symptoms begin a few months after menarche | Symptoms begin years after menarche, especially after 25 years |
| Pain begins before or on the 1st day of menstruation and lasts from 8 hours to 3 days | Pain can arise at any stage of menstruation, the intensity can vary from day to day |
| Nausea, vomiting, headache are present | Bleeding and pain during or after intercourse, plus heavy menstruation may be present |
| No change in exams | Exams point to pelvic diseases |
| Normal family history with no relevant changes in the woman | History of endometriosis in the family, previously detected STD, IUD use, internal absorbent or pelvic surgery already performed |
Furthermore, in primary dysmenorrhea, it is common for symptoms to be controlled by taking anti-inflammatories and oral contraceptives, whereas in secondary dysmenorrhea there are no signs of improvement with these medications.
Symptoms and diagnosis of dysmenorrhea
Severe menstrual cramps may appear a few hours before menstruation, and other symptoms of dysmenorrhea are also present, such as:
- Nausea;
- Vomiting;
- Diarrhea;
- Fatigue;
- Pain in the back;
- Nervousness;
- Dizziness;
- Severe headache.
The psychological factor also seems to increase levels of pain and discomfort, compromising even the effect of pain relief remedies.
The gynecologist is the most appropriate doctor to make the diagnosis after hearing the woman's complaints, and the intense colic in the pelvic region during menstruation is especially valued.
To confirm the doctor usually palpates the uterine region to check if the uterus is enlarged and asks for tests such as abdominal or transvaginal ultrasound to discover diseases that may be causing these symptoms, which is crucial to determine if it is a primary or secondary dysmenorrhea, in order to indicate the appropriate treatment for each case.

How to treat dysmenorrhea to end pain
Medicines
To treat primary dysmenorrhea it is recommended to use analgesic and antispasmodic drugs, such as Atroveran compound and Buscopan, under the indication of the gynecologist.
In the case of secondary dysmenorrhea, the gynecologist may indicate the use of non-hormonal analgesic or anti-inflammatory drugs, such as mefenamic acid, ketoprofen, piroxicam, ibuprofen, naproxen for pain relief, as well as medicines that reduce menstrual flow such as Meloxicam, Celecoxib or Rofecoxib.
Learn more about Treatment for Dysmenorrhea.
Natural Treatment
Some women benefit by putting a warm thermal gel bag over their belly. Relaxing, taking a warm bath, relaxing massages, exercising 3 to 5 times a week, and not wearing tight clothing are some other suggestions that usually bring pain relief.
Decreasing salt intake 7 to 10 days before menstruation also helps to combat pain by decreasing fluid retention.