Bacterioscopy is a diagnostic technique that allows to identify quickly and in a simple way the occurrence of infections, because by means of specific staining techniques, it is possible to visualize the bacterial structures in the microscope.
This test can be done with any biological material, and the doctor must indicate the material to be collected and analyzed, and the result indicates whether the presence or absence of bacteria, as well as their quantity and characteristics have been verified.

What is it for
Bacterioscopy is a diagnostic test that can be done with any biological material and can be used to quickly identify bacterial infections:
- Sexually transmitted diseases such as gonorrhea and chlamydia, for example, penile or vaginal secretions being used for this purpose. The collection is done through the use of a sterile swab and it is contraindicated to carry out the hygiene of the genital region 2 hours before the examination and nor to have sex in the 24 hours before the collection;
- Tonsillitis, because through the collection of throat secretions, it is possible to identify gram-positive bacteria responsible for inflammation in the amygdala, with the presence of streptococcal bacteria;
- Infections in the urinary system, which is done by analyzing the first jet of urine;
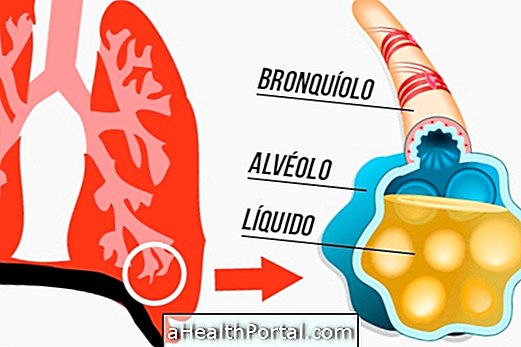
- Tuberculosis, in which the sputum is analyzed;
- Infections in surgical wounds, since it is common that infections occur after operations due to the diminution of the immune system of the person. Thus, collection of wound secretion with a sterile swab may be indicated to verify the possible presence of bacteria in the site;
- Skin or nail injuries, which consists of the collection of a superficial sample, not to use creams and enamels at least 5 days before the examination. Although bacterioscopy can be performed, fungi are usually observed when examining the nail sample, for example.
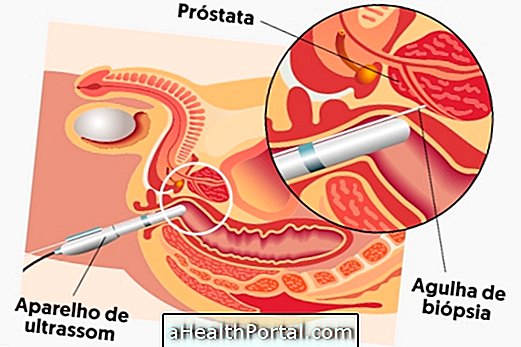
In addition, bacterioscopy may be used to aid in the diagnosis of bacterial meningitis, respiratory and gastrointestinal tract diseases, and may be done by biopsy or anal material.
Thus, bacterioscopy is a laboratory technique that can be used in clinical practice to diagnose diseases caused by bacteria, indicating the characteristics of the causative agent of the disease and thus allowing the physician to start the treatment even before being identified in the laboratory, which can take about 1 week.

How is it done?
The bacterioscopy examination is done in the laboratory and the material collected from the patient is analyzed in the microscope to investigate the absence or presence of bacteria, in addition to its characteristics.
The preparation to take the exam depends on the material that will be collected and analyzed. In the case of vaginal material, it is not recommended for the woman to hygienize 2 hours before the examination and not to have intercourse in the last 24 hours, whereas in the case of collection of nail or skin material, for example, it is recommended not to pass enamel, creams or substances on the skin prior to examination.
In the case of a sample of vaginal secretion, for example, the swab that was used to make the collection is passed in circular motions on a slide, which must be identified with the patient's initials, and then stained with the Coloring of Gram. In the case of a sputum sample, for example, which is the material collected mainly to verify the presence of the bacterium responsible for tuberculosis, the staining used in bacterioscopy is that of Ziehl-neelsen, which is more specific for this type of microorganism.
Normally when the presence of bacteria is verified, the laboratory performs the identification of the microorganism and the antibiogram, giving a more complete result.
How is Gram stain made?
The staining of gram is a simple and fast coloring technique that allows the differentiation of bacteria according to their characteristics, allowing differentiation of bacteria into positive or negative according to their coloring, allowing their visualization under the microscope.
This staining method uses two main dyes, one blue and one pink, which may stain the bacteria or not. Bacteria stained in blue are said to be gram-positive, while those in pink are called gram-negative. From this classification, it is possible that the doctor starts the preventive treatment, even before the identification of the microorganism.
Understand how Gram stain is made
Bacterial identification by means of gram staining is quick, practical and inexpensive to make, and is essential for physicians since specific characteristics of these groups of bacteria are known and the doctor can indicate a preventive treatment based only on staining of gram.
This coloring has as principle the differentiation of bacteria according to the characteristics of the cell wall. Gram-positive bacteria have more than one thick wall of peptideoglycan, being able to retain the first dye well, while gram-negative bacteria have a thinner wall and can be easily discolored when exposed to alcohol.
Gram staining is done in 5 main steps, but the protocol may vary according to the laboratory:
- Cover the blade with the violet crystal dye and allow to act for about 1 minute;
- Wash the blade with a stream of running water and cover the blade with lugol, which aims to fix the blue dye, and leave to act for 1 minute. Both types of bacteria can absorb the complex formed by dye and lugol, turning blue;
- Then wash the blade with running water and apply 95% alcohol, letting it act for 30 seconds. Alcohol is responsible for dissolving the lipid membrane which forms the gram-negative bacteria and thereby removing the complex formed between the dye and the lugol, discoloring those bacteria. However, in the case of gram-positive bacteria, alcohol is depleted of the cell wall of gram-positive bacteria, causing contraction of the pores and rendering them impermeable;
- Then rinse under running water and cover the blade with the second dye, fuchsin or safranine and allow to act for 30 seconds;
- The blade should then be rinsed with tap water and allowed to dry at room temperature.
Once the blade is dry, it is possible to place a drop of immersion oil and observe the blade in the microscope with a 100x objective. It is possible to verify the presence or presence of bacteria, as well as the presence of yeasts and epithelial cells.
What does the result mean?
The aim of the bacterioscopy result is to indicate if there is presence or absence of microorganisms, characteristics and quantity, besides the material that was analyzed.
The result is said negative when no microorganisms are observed and positive when microorganisms are visualized. The result is usually indicated in crosses (+), where 1 + indicates that 1 to 10 bacteria were visualized in 100 fields and could be indicative of an initial infection, for example, and 6 + represents the presence of more than 1000 bacteria per observed field, representing a more chronic infection or bacterial resistance, for example, indicating that the treatment is not being effective.
In addition, the coloring information that has been used in the report is known, which may be Gram or Ziehl-neelsen, for example, in addition to the characteristics of the microorganism, as a form and arrangement, whether in clusters or in chains, for example.
Normally, when the result is positive, the laboratory identifies the microorganism and antibiogram, indicating which antibiotic is most recommended to treat infection by a certain bacterium.