The loop test is a quick examination that helps identify blood vessel fragility and bleeding tendency, common in diseases such as dengue, scarlet fever or thrombocytopenia, for example. During the examination, small red spots appear on an area of the arm after obstruction of the blood flow with a tourniquet, and the larger the amount, the greater the risk of herring.
Also known as tourniquet test, Rumpel-Leede test or capillary fragility test, this test is fast and practical, so it is part of the World Health Organization recommendations for the diagnosis of dengue, although this test is not always positive in people with dengue.
As it identifies the risk of bleeding, the loop test does not need to be used when there are already signs of bleeding, such as bleeding gums, nose or urine. In addition, the loop test may show false results in situations such as aspirin, corticosteroids, pre or postmenopausal phase, or sunburn, for example.

How is it done?
To test the loop, a square with an area of 2.5 x 2.5 cm should be drawn on the forearm and then follow these steps:
- Assess the person's blood pressure with the sphygmomanometer;
- Re-inflate the sphygmomanometer cuff to the mean value between maximum and minimum pressure. The calculation is made by the formula: Maximum Blood Pressure + Minimum Blood Pressure divided by 2, that is, if the blood pressure value is 120x80, the cuff should be inflated to 100 mmHg;
- Wait 5 minutes with the cuff inflated to the same pressure;
- After 5 minutes deflate and remove the cuff ;
- Let the blood circulate for at least 2 minutes.
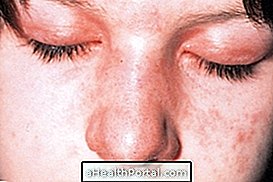
Finally, the amount of red spots, called petechiae, should be evaluated inside the square on the skin to know the result of the test.
When the result is positive
The loop test result is considered positive when more than 20 red dots appear within the square marked on the skin. However, a result with 5 to 19 spots may already indicate suspicion of dengue, and other tests should be done to help confirm whether or not the infection is present.
It is important to remember that the examination may be false negative even in people who have the disease, so if suspected, the doctor should ask for further evaluations to confirm. In addition, it can be positive in other diseases that cause capillary fragility and risk of bleeding, such as other infections, diseases of immunity, genetic diseases or even, use of medicines such as aspirin, corticoid and anticoagulants, for example.
Thus, it can be observed that this examination is not specific and should be done only to aid in the diagnosis of dengue. Learn more about the other causes of bleeding on the skin.
What other tests may be needed
To assist in the diagnosis of dengue, the physician should also make the clinical evaluation of the affected person and may request other more specific tests to assist in the diagnosis, which include:
- Rapid test (NS1);
- Serology for dengue;
- Hemogram (with platelet count to assess the risk of bleeding).
See the main symptoms that may indicate a dengue infection.