Most intestinal infarcts happen when an artery, which carries blood into the intestine, is blocked by a clot and stops the passage of blood with oxygen to the sites that remain after the clot, leading to the death of that part of the intestine and generating symptoms such as severe belly pain, vomiting and fever, for example.
In addition, bowel infarction may also occur in a vein in the region of the mesentery, which is the muscle that holds the bowel. When this happens, the blood can not get out of the intestine into the liver, and therefore the blood with oxygen can not continue to circulate in the intestine, resulting in the same consequences as the infarct of the artery.
Intestinal infarction has a cure, but it is an emergency situation, so if there is suspicion it is very important to go to the emergency room quickly to confirm the diagnosis and start the appropriate treatment so that a large portion of the intestine is affected.

Main symptoms
The most frequent symptoms in the case of infarct of the intestine include:
- Severe abdominal pain that worsens over time;
- Feeling of swelling in the belly;
- Nausea and vomiting;
- Fever above 38ºC;
- Diarrhea with blood in the stool.
These symptoms may appear suddenly or develop slowly over several days, depending on the size of the region affected by ischemia and the severity of the obstruction.
That way, if there is a very intense abdominal pain that does not improve after 3 hours, it is very important to go to the hospital to identify the problem and start the appropriate treatment, since it can be a bowel infarction.
How to confirm the diagnosis
To make the diagnosis of intestinal infarction, your doctor may order various tests such as magnetic resonance imaging, ultrasound, X-ray, blood tests, and even endoscopy or colonoscopy to ensure that the symptoms are not being triggered by other digestive tract problems such as ulcers or appendicitis, for example.

How is the treatment done?
Treatment for infarct in the gut is almost always done with surgery to remove the clot and restore blood flow in the affected vessel, in addition to removing any portion of intestine that has been affected.
Before surgery, your doctor may stop using medicines that may be contracting blood vessels, such as migraine medicines, to treat heart disease, and even some types of hormones.
In some cases, antibiotics may still need to be done before and after surgery to prevent the development of infections in the affected bowel.
Sequelae of intestinal infarction
One of the most common sequelae of ischemia in the gut is the need to have an ostomy. This is because, depending on the amount of bowel removed, the surgeon may not be able to reconnect the intestine to the anus, so it is necessary to make a connection directly to the belly skin, allowing the stool to exit into a small pouch.
In addition, with the removal of intestine, the person also has short bowel syndrome that, depending on the part withdrawn, causes difficulty in absorption of some vitamin and minerals, and it is important to adjust the diet. See more about this syndrome and what the diet should be like.
Possible Causes of Intestinal Infarction
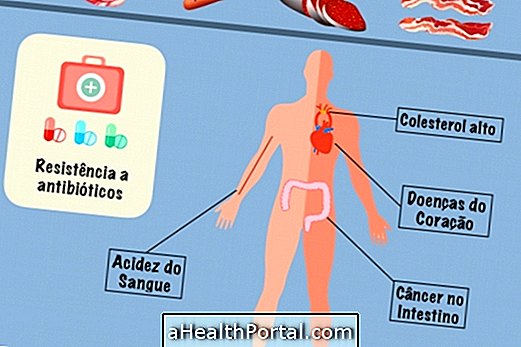
Although intestinal infarction is a very rare condition, there is a greater risk in people with:
- Age greater than 60 years;
- High cholesterol levels;
- Ulcerative colitis, Crohn's disease or diverticulitis;
- Cancer in the digestive system.
In addition, women who use contraceptive pills also have an increased risk of clot formation and, therefore, may develop a case of infarct in the gut.