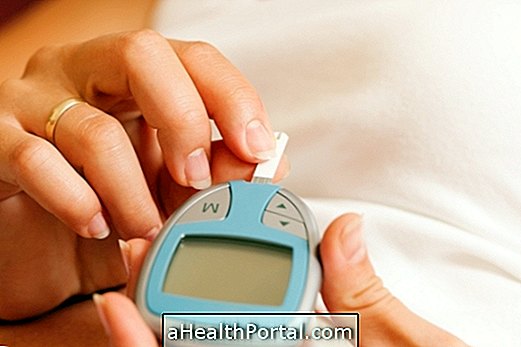
Gestational diabetes usually develops near the third trimester of pregnancy due to insulin resistance caused by the gestational hormones. This type of diabetes usually goes away after birth and rarely causes symptoms, although in some cases blurred vision and thirst may occur.
Your treatment should be started even during gestation with an adequate diet or with the use of medicines, such as oral hypoglycemic agents or insulin, depending on blood sugar values.
However, it is important to correctly follow the treatment proposed by the doctor, since there is a high risk of developing type 2 diabetes mellitus in about 10 to 20 years and also of suffering from diabetes in another pregnancy.
Main symptoms
The symptoms of gestational diabetes are not easily perceived, as many are confused with the common pregnancy changes, such as:
- Excessive hunger;
- Very thirst;
- Exaggerated weight gain in woman or baby;
- Increased urge to urinate;
- Extreme fatigue;
- Swelling in the legs and feet;
- Blurred vision;
- Candidiasis or frequent urinary tract infection.
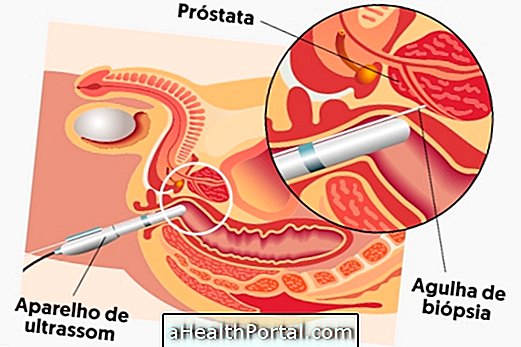
As these symptoms are common in pregnancy the doctor should request the glucose test at least 3 times during gestation and usually the first examination is done at 20 weeks. For diagnosis, the obstetrician may request tests such as:
- Fasting glycemia: not to exceed 85 mg / dl in the pregnant woman;
- Examination of the glycemic curve from 22 weeks of gestation.
In the case of identifying the disease, the pregnant woman is submitted to glycemic control in short and regular interval visits. See how the gestational diabetes test is done.
How is the treatment done?
Treatment for gestational diabetes is usually started only with a low-carbohydrate diet and regular practice of moderate exercise.
However, in more severe cases where the amount of blood sugar is much higher than expected, one should choose to use oral hypoglycemic drugs or insulin in order to control blood sugar by keeping it under acceptable rates. Oral hyperglycemic agents, such as Metformin, should not be used in pregnancy, but there are others that may be prescribed by your doctor.
How is the diet for gestational diabetes?
In this type of diet it is advised to eat foods with low glycemic index, such as peeled fruits, as well as decrease the amount of sugar and carbohydrates from the food. That way, the pregnant woman can not eat sweets, fried foods, soda, processed juices, butter and chocolate, for example. Check out all the care you should take in feeding.
See our nutritionist tips:
Possible Complications
The complications of gestational diabetes can affect the pregnant woman or the baby, and may be:
| Risks for pregnant women | Risks for the baby |
| Amniotic pouch rupture ahead of schedule | Development of respiratory distress syndrome, which is difficulty breathing at birth |
| Premature birth | A baby too large for gestational age, which increases the risk of obesity in childhood or adolescence |
| Fetus that does not turn upside down before delivery | Heart diseases |
| Increased risk of preeclampsia, which is the sudden rise in blood pressure | Jaundice |
| Possibility of cesarean delivery or laceration of the perineum in normal delivery due to the size of the baby | Hypoglycemia after birth |
These risks can be lowered if the woman follows the treatment correctly, so the pregnant woman with gestational diabetes should be followed up at high risk prenatal care.
How to prevent gestational diabetes
Gestational diabetes can not always be prevented because the hormonal changes typical of pregnancy are related; however, the risk of developing gestational diabetes can be reduced by:
- Being at the ideal weight before becoming pregnant;
- Do the prenatal care;
- Increase weight slowly and gradually;
- Eat healthy and
- Practice moderate exercise.
Gestational diabetes may occur in pregnant women over 25 years old, obese or when the pregnant woman has an intolerance to sugars. However, it can also develop in younger or normal-weight women due to hormonal changes.