Mitral valve prolapse, in most women, does not present complications during pregnancy, delivery or the baby. However, when associated with other heart diseases such as major mitral regurgitation, pulmonary hypertension, atrial fibrillation and infective endocarditis, more care and follow-up is required by an obstetrician and cardiologist with experience in high-risk pregnancies.
Treatment for mitral valve prolapse in pregnancy
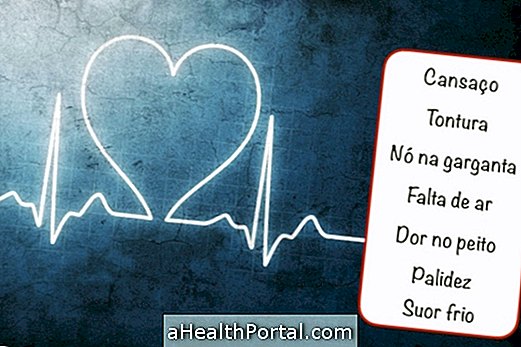
Treatment for mitral valve prolapse in pregnancy is only necessary when symptoms such as chest pain, tiredness or difficulty breathing are manifested.
Treatment in such cases should always be done with the follow-up of a cardiologist and, preferably, a specialist in heart disease during pregnancy, who may prescribe:
- Antiarrhythmics: control irregular heartbeats;
- Diuretics: help remove excess fluid from the lungs;
- Anticoagulants: help prevent blood clots.
In some cases, antibiotics may be needed during delivery to avoid the risk of mitral valve infection, but as much as possible, the use of medications during pregnancy should be avoided.
Care in Prolapse of the Mitral Valve in Pregnancy
Care in mitral valve prolapse in pregnancy is simple but important and involves:
- Rest and restraint of physical activity;
- Weight gain <10 kg;
- Iron supplements after the 20th week;
- Decreased consumption of salt.
In general, mitral valve prolapse in pregnancy is well tolerated and the mother's body adapts well to the overload of the pregnancy's own cardiovascular system.
Does mitral valve prolapse hurt the baby?
Mitral valve prolapse only damages the baby in more severe cases, where it is necessary to perform surgery for repair or replacement of the mitral valve. These procedures are usually safe for the mother, but for the baby can represent a risk of death between 2 to 12% and is therefore avoided during pregnancy.
Useful links:
Mitral valve prolapse