Lupus is a chronic, autoimmune inflammatory disease that, although it has no cure, can be controlled with the use of medicines that help decrease the action of the immune system, such as corticosteroids and immunosuppressants, and care such as the application of sunscreen daily for example, according to the guidelines of the rheumatologist or dermatologist, which helps to control and avoid crises, according to the manifestations of the disease in each person.
All patients with lupus need medical follow-up, but the disease is not always active, and it is usually possible to maintain normal day-to-day activities, such as working or carrying out leisure activities, for example.
The main symptoms that arise in this disease include red patches on the skin, especially in areas exposed to light such as face, ears or arms, hair loss, low fever, loss of appetite, pain and swelling of the joints and malfunction of the kidneys, for example . See the full list of lupus symptoms to identify this disease.

How To Control Lupus
Although lupus has no cure, the disease can be controlled by follow-up with the rheumatologist, who will guide the use of remedies to decrease inflammation, which varies according to the type of disease, the organs affected, and the severity of each case. The treatment options, which are also available by SUS, are:
1. Sun protection
The use of sunscreen with SPF of at least 15, but preferably above 30, is an important way of avoiding the formation of cutaneous lesions present in discoid or systemic type lupus with cutaneous manifestations. The sunscreen or sunscreen should always be applied in the morning, and reapplied at least once more throughout the day, depending on local lighting and the possibility of exposure.
In addition, the use of clothing and hats are important to prevent the action of ultraviolet rays on the skin when in sunny environments.
2. Analgesics and anti-inflammatories
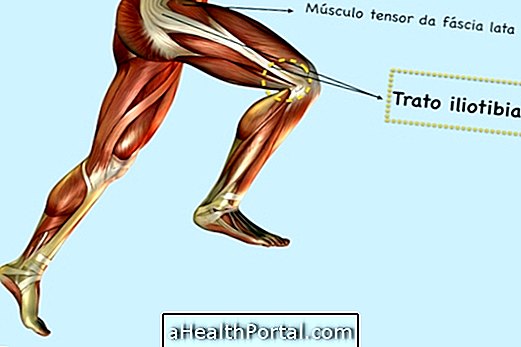
Pain-relieving medicines may be anti-inflammatory drugs, such as Diclofenac, or analgesics, such as Paracetamol, which are very useful for times when pain control is needed, especially when the disease affects the joints.
3. Corticosteroids
Corticosteroids, or corticosteroids, are medicines that are often used to control inflammation. They may be of topical use in ointments used in skin lesions to aid in their improvement and make it difficult to increase the size of wounds and blisters.
They are also used in oral tablet form in cases of both mild and severe lupus or situations of exacerbation of the systemic disease, where there may be damage to blood cells, kidney function, or involvement of organs such as the heart, lungs and lungs. nervous system, for example.
The dose and the time of use depend on the severity of the situation, for each case. In addition, there is the option of injectable corticosteroids, most often used in severe cases or where there is difficulty in swallowing the tablet.
4. Other immunity regulators
Some medicines that can be used in conjunction with corticosteroids or used separately for disease control are:
- Antimalarials, such as Chloroquine, especially in joint disease, are useful for both systemic and discoid lupus, even in the remission phase to keep the disease under control;
- Immunosuppressants, such as Cyclophosphamide, Azathioprine or Mycophenolate mofetil, for example, are used with or without corticosteroids to weaken and soothe the immune system for more effective control of inflammation;
- Immunoglobulin, is an injectable drug, made in severe cases in which there is no improvement of the immunity with other medicines;
- Biological agents, such as Rituximab and Belimumab, are new drugs genetically engineered products, also reserved for severe cases where there is no improvement with other alternatives.

5. Natural Options
Some day-to-day attitudes, practiced at home, along with treatment, are also important to help keep the disease under control. Some options are:
- Do not smoke;
- Avoid alcoholic beverages;
- Practice physical activity 3 to 5 times a week, during periods of remission of the disease;
- Make a diet rich in omega-3, present in salmon and sardines, for example, 3 times a week;
- Consume foods that are anti-inflammatory and photo-protective like green tea, ginger and apple, for example in addition to other types of fruits, vegetables and greens.
Check out this video, with more options and tips, to know how to eat well and live better with this disease:

In addition, it is essential to maintain a balanced diet, avoiding the consumption of foods rich in sugar and fat, as they contribute to the increase of triglycerides, cholesterol and sugar levels, which can cause weight gain and diabetes, which can disease.
Other precautions include avoiding live virus vaccines except under medical indication, monitoring calcium and vitamin D levels in the blood, which may decrease with the use of corticosteroids, physical therapy to prevent and treat joint pain, and prevent stress, which can influence the outbreaks of the disease.
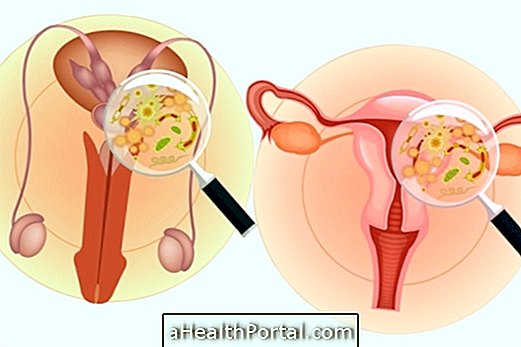
Caring for lupus in pregnancy
It is possible to become pregnant when you have lupus; however, it should preferably be a planned pregnancy at a less severe time of the disease and should be monitored throughout the period by the obstetrician and rheumatologist due to the possibility of exacerbation of the disease.
In addition, the medications are adjusted for gestation and during breast-feeding so that it is the least toxic possible for the baby, usually with the use of corticosteroids in low doses.