Hepatitis B in pregnancy is dangerous because there is a high risk of the pregnant woman infecting the baby at the time of delivery.
However, contamination can be avoided if the woman takes the vaccine against hepatitis B before becoming pregnant, or from the second trimester of gestation. In addition, soon after birth, the baby should take the vaccine and immunoglobulin injections to fight the virus and thus not develop hepatitis B.
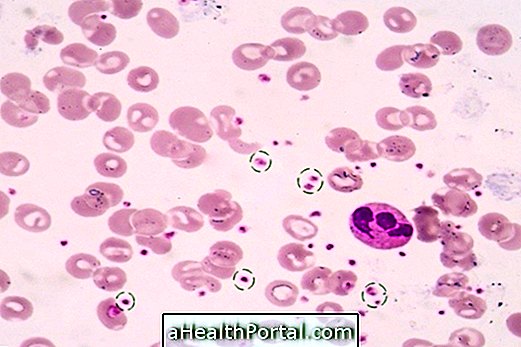
Hepatitis B, during pregnancy, can be diagnosed through an HbsAg and anti-HBc blood test, which is part of prenatal care. Once confirmed that the pregnant woman is infected, she should consult a hepatologist to indicate the appropriate treatment, which can be done only with rest and diet or with herbal remedies depending on the severity and stage of the disease.

How to treat hepatitis B in pregnancy
Treatment of acute hepatitis B in pregnancy includes rest, hydration, and a low-fat diet, which aid in liver recovery. To prevent contamination of the baby, your doctor may suggest vaccines and immunoglobulins.
In case of chronic hepatitis B in pregnancy, even if the pregnant woman does not present any symptoms, the doctor may prescribe the use of some doses of Lamivudine to reduce the risk of contamination of the baby.
Together with Lamivudine, the doctor may prescribe immunoglobulin injections for the pregnant woman to take in the later months of pregnancy to lower the viral load in the blood and thus decrease the risk of infecting the baby. However, this decision is made by the hepatologist, who is the specialist who should indicate the best treatment.
Risks of hepatitis B in pregnancy
The risks of hepatitis B in pregnancy can occur for both the pregnant woman and the baby:
Risks for pregnant women
The pregnant woman, when not treated for hepatitis B and not following the guidelines of the hepatologist, may develop serious liver diseases, such as liver cirrhosis or liver cancer, suffering damage that may be irreversible.
Risks for the baby
Hepatitis B in pregnancy is usually transmitted to the baby at the time of delivery through contact with the mother's blood, and in rare cases it is also possible to have contamination through the placenta. Therefore, soon after birth, the baby should receive a dose of the hepatitis B vaccine and an immunoglobulin injection up to 12 hours after giving birth and two more doses of the vaccine at the 1st and 6th month of life.
Breastfeeding can be done normally, since the hepatitis B virus does not pass through breast milk.

When to take the hepatitis B vaccine
All women who did not take the hepatitis B vaccine and who are at risk of developing the disease should take the vaccine before pregnancy to protect themselves and the baby.
Pregnant women who have never taken the vaccine or who have an incomplete schedule can take this vaccine during pregnancy from 13 weeks of gestation because it is safe.
Learn more about the hepatitis B vaccine.
How to ensure your baby will not be contaminated
To ensure that the baby, the child of an acute or chronic hepatitis B mother, is not infected, it is recommended that the mother follow the treatment proposed by the doctor and that the baby immediately after birth takes the hepatitis B vaccine and injections of hepatitis B specific immunoglobulin.
About 95% of babies who are treated in this way at birth do not become infected with the hepatitis B virus.
Signs and symptoms of hepatitis B in pregnancy
Signs and symptoms of acute hepatitis B in pregnancy include:
- Skin and yellow eyes;
- Numbness;
- Vomiting;
- Tiredness;
- Pain in the abdomen, especially in the upper right, where the liver is located;
- Fever;
- Lack of appetite;
- Clear stools, such as putty;
- Dark urine, like the color of coca cola.
In chronic hepatitis B, the pregnant woman usually has no symptoms, although this situation also poses risks for the baby.
Learn all about hepatitis B.