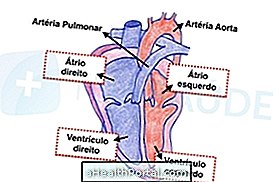
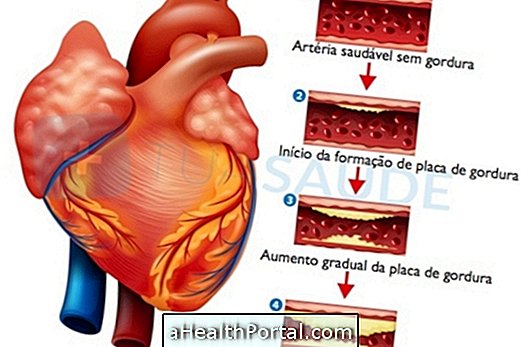
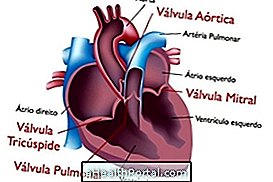
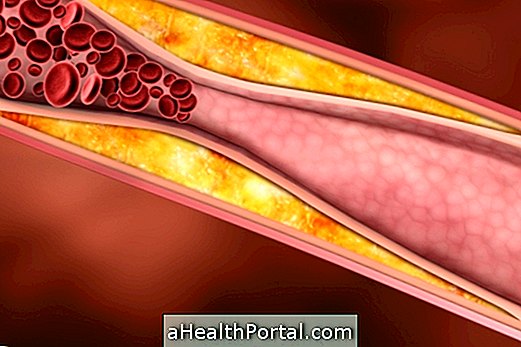
Cardiac ischemia or myocardial ischemia is characterized by decreased blood flow through the coronary arteries, which are vessels that carry blood to the heart. It is usually caused by the presence of fat plaques inside it, which when not properly treated can rupture and clog the vessel, causing pain and increasing the chances of a heart attack.
Its treatment is made with medicines to improve the blood flow of these vessels, prescribed by the cardiologist, such as metoprolol, simvastatin and AAS, for example, besides the control of cholesterol and salt in the diet and physical activity.

Types of cardiac ischemia
Obstruction of coronary blood flow can occur in different ways:
- Stable angina : is a type of chronic, but transient ischemia because chest pain arises when the person makes some effort, suffers some emotional stress or after eating, and improves in a few minutes or when he rests. If left untreated, it could be a heart attack in the future.
- Unstable angina is also a type of chronic ischemia, but chest pain can occur at any time, lasts longer than 20 minutes, does not improve with rest, and if not quickly treated, will progress to a heart attack. Understand better what angina is, its causes and how to treat.
- Acute myocardial infarction : infarction may occur after angina transformation, or it may be sudden, arising unannounced. It is characterized by intense pain or burning in the chest that does not improve and should be treated as soon as possible in the emergency room. Learn how to identify a heart attack.
- Silent ischemia is the reduction of coronary blood flow that causes no symptoms, is often discovered in routine exams, and causes a high risk of progression to a sudden cardiac arrest or cardiac arrest.
These types of ischemia cause a great compromise in the health of the heart, so they should be diagnosed and treated as soon as possible, either by performing annual check-ups or by seeking care from a general practitioner or cardiologist whenever symptoms of pain appear or burning in the chest.
How is the treatment done?
Treatment for cardiac ischemia can be done with the use of medications to:
- Reduce heart rate, such as propranolol, atenolol or metoprolol;
- Controlling blood pressure levels, such as enalapril, captopril, or losartan;
- Reduce fat plaques, such as simvastatin and atorvastatin;
- Decrease the formation of blood clots, such as AAS or clopidogrel, to break down fat plaques;
- Dilate the vessels of the heart, such as isordil and monocordil.
These medicines should only be used under the strict guidance of the cardiologist. It is also important to control diseases such as high cholesterol, high blood pressure, smoking, sedentary lifestyle, diabetes, sleep apnea and anxiety attacks, as they may increase the risk of cardiac ischemia.
In more severe cases, when the use of medication is not enough, the cardiologist may indicate the surgery, which is a delicate procedure in which the patient can stay in the hospital for more than 4 days and must perform physiotherapy still in the hospital for rehabilitation cardiac disease. The doctor may, for example, request angioplasty with or without a stent or myocardial revascularization surgery, which is the replacement of a coronary by the saphenous vein, for example. Understand how the saphenous vein surgery is done.

Symptoms of cardiac ischemia
Symptoms of cardiac ischemia may be:
- Pain or burning in the chest that can radiate to the nape of the neck, chin, shoulders or arms;
- Heart palpitations;
- Chest pressure;
- Shortness of breath or difficulty breathing;
- Numbness, cold sweat, pallor and malaise;
However, cardiac ischemia may not show symptoms being only discovered on a routine examination or when it causes a heart attack. See which are the 12 signs that can indicate problems in the heart.
Causes of cardiac ischemia
The main cause of cardiac ischemia is atherosclerosis, which is the accumulation of fat inside the coronary arteries, due to the long-term effect of high cholesterol, high sugar, sedentary lifestyle, smoking and obesity.
However, other diseases can lead to cardiac ischemia such as lupus, diabetes, coronary embolism, syphilis, aortic stenosis, coronary spasm, very severe hyperthyroidism and use of drugs such as cocaine and amphetamines.
How is the diagnosis made?
To identify the presence of ischemia in the heart, some tests may be done, which should be requested by the general practitioner or cardiologist, such as:
- Electrocardiogram;
- Exercise test or stress test;
- Echocardiography;
- Myocardial scintigraphy.
Blood tests are performed to identify the presence of changes that cause risk to the heart, such as cholesterol, glycemia, triglycerides and renal function, for example. When suspected infarction, blood test to assess levels of cardiac enzymes may also help confirmation. Find out what tests are required to evaluate the heart.
Each examination requested depends on the person's symptoms, and if there is still any doubt, the cardiologist may request a cardiac catheterization to confirm the presence of cardiac ischemia. Find out what it is for, how it is done and the risks of cardiac catheterization.