Pressure ulcer, also popularly known as eschar, is a wound that appears due to prolonged pressure and consequent decrease in blood circulation in a certain part of the skin.
This type of wound is more common in places where the bones are in greater contact with the skin, such as the bottom of the back, the neck, the hip or the heels, because there the pressure on the skin is greater, worsening circulation. In addition, pressure ulcers are also more common in bedridden people, as they can spend several hours in a row in the same position, which also makes it difficult to circulate in some places on the skin.
Although pressure sores are skin sores, they take a long time to heal and this happens for several reasons, such as weakness of the person's general condition, alteration of the deep layers of the skin and difficulty in completely relieving all the pressure from the affected places. Therefore, it is very important that all types of ulcers are evaluated by a doctor or a nurse, so that treatment with the most appropriate product can be started, as well as the most important care to speed up healing is explained.

Main stages of pressure ulcer
Initially, pressure ulcers appear on the skin only as a red spot, but over time this spot may present a small wound that does not heal and that increases in size. Depending on the moment of the ulcer evolution, it is possible to identify 4 stages:
Stage 1
The first stage of pressure ulcers is known as "blanching erythema" and means that, at first, the ulcer appears as a reddish spot that when pressed changes color to white or becomes paler, and that maintains that coloration during a few seconds or minutes, even after the pressure has been removed. In the case of black or darker skin, this spot may also have a dark or purplish color, instead of red.
This type of stain, in addition to being white for a long time after being pressed, can also be harder than the rest of the skin, be hot, or else be cooler than the rest of the body. The person may also refer to the sensation of tingling or burning in that place.
What to do: at this stage, pressure ulcers can still be prevented and, therefore, the ideal is to keep the skin intact and improve blood circulation. For this, one should try to keep the skin as dry as possible, apply a moisturizing cream frequently, as well as avoid positions that can put pressure on the place for more than 40 minutes in a row. In addition, it is important to have regular massages on site to facilitate circulation.
Stage 2
At this stage, the first wound appears, which may be small, but which appears as an opening of the skin in the region of the blotchy erythema stain. In addition to the wound, the skin in the area of the stain appears thinner and may look dry or else be brighter than normal.
What to do: although the wound has already appeared, at this stage it is easier to stimulate healing and prevent infection. For that, it is important to go to the hospital, or to a health center, so that the place is evaluated by a doctor or nurse, in order to start the treatment with the most appropriate products and dressings. In addition, you should continue to relieve the pressure of the site, so as to drink a lot of water and increase the intake of foods rich in protein and vitamins, such as egg or fish, as they facilitate healing.

Stage 3
In stage 3, the ulcer continues to develop and increase in size, beginning to affect deeper layers of the skin, including the subcutaneous layer, where the fat deposits are found. That is why, at this stage, inside the wound it is possible to observe a type of irregular and yellowish tissue, which is formed by fat cells.
At this stage, the depth of the ulcer varies according to the affected site and, therefore, it is normal that in the nose, ears or ankles it is not possible to observe the subcutaneous layer, since it is not present.
What to do: Adequate treatment must be maintained with the guidance of a nurse or doctor, and it is necessary to make a closed dressing every day. It is important to drink plenty of water during the day and bet on the most protein-rich diet. In addition, you should also continue to relieve the pressure of the affected places, and it may even be recommended by the doctor to buy a mattress that varies the pressure along the body, especially in people who are bedridden for a long time.
Stage 4
This is the last stage of development of the pressure ulcer and is characterized by the destruction of the deeper layers, where the muscles, tendons and even the bones are found. In this type of ulcers there is a high risk of infection and, therefore, the person may need to be hospitalized to make more regular dressings and receive antibiotics directly into the vein.
Another very common characteristic is the presence of a very foul smell, due to the death of the tissues and the production of secretions that can become infected.
What to do: These ulcers must be treated in the hospital and it may even be necessary to stay in hospital to make antibiotics and prevent a possible infection. It may also be necessary to remove layers of dead tissue, and surgery may be recommended.
Main nursing care
One of the most important nursing care in the case of pressure ulcers is to perform an adequate dressing, however, the nurse must also maintain a regular assessment of the wound, as well as teach the person to avoid the worsening of the ulcer and assess the risk of new ulcers.
1. How to heal the ulcer
The dressing should always be adapted to the type of tissue present in the wound as well as other characteristics that include: release of secretions, smell or presence of infection, in order to promote adequate healing.
Thus the dressing can include different types of material, the most common of which include:
- Calcium alginate: foams widely used in pressure ulcers to absorb released secretions and form an ideal environment for healing. They can also be used if there is bleeding, as they help to stop bleeding. Usually, they need to be changed every 24 or 48 hours.
- Silver alginate: in addition to absorbing secretions and promoting healing, they also help to treat infections, being a good option for infected pressure ulcers;
- Hydrocolloid: it is ideal to prevent the appearance of the wound even during stage 1 of the pressure ulcer, but it can also be used in the more superficial ulcers of stage 2;
- Hydrogel: can be used in the form of a dressing or gel and helps remove dead tissue from the wound. This type of material works best on ulcers with little secretion;
- Collagenase: is a type of enzyme that can be applied to the wound to degrade dead tissue and facilitate secretion, being widely used when there are large areas of dead tissue to remove.
In addition to using the appropriate dressing, the nurse must remove the remains of the previous dressing and clean the wound properly where, in addition to using saline, a scalpel can be used to remove pieces of dead tissue, which is called debridement. . This debridement can also be done directly with the compress during cleaning or done with the application of enzymatic ointments, such as collagenase.
Check out more about ointments for the treatment of pressure ulcers.

Most common pressure ulcer sites
2. How to assess pressure ulcers
During the treatment of the wound, the nurse must be attentive to all the characteristics that he can observe or identify, so that an assessment can be made over time, in order to understand if an adequate healing is taking place. This evaluation is also very important to consider changing the dressing materials, so that they remain adequate throughout the treatment.
Some of the most important characteristics, which should be evaluated during all dressings include: size, depth, shape of the edges, production of secretions, presence of blood, smell and presence of signs of infection, such as redness in the surrounding skin, swelling, heat or pus production. Sometimes, the nurse can even take photographs of the wound site or make a drawing with a paper under the wound, to compare the size over time.
When evaluating the characteristics of pressure ulcers, it is also recommended to pay attention to the skin around the wound, since if it is not properly hydrated, it can contribute to the increase of the ulcer.
3. What to teach the person with pressure ulcers
There are several teachings that are very important for the person with pressure ulcers and that can help to greatly improve the speed of healing, as well as avoid complications. Some of these teachings include:
- Explain to the person the importance of not staying in the same position for more than 2 hours;
- Teach the person to position so as not to apply pressure on the ulcer;
- Show how to use pillows to relieve pressure on bone sites;
- Teach about the harm of smoking to blood circulation and encourage the person to stop smoking;
- Explain about the signs of possible complications, especially infection.
In addition, it may also be important to refer the person to a consultation with a nutritionist, since proper nutrition is very important to promote the formation of collagen and the closure of the wound.
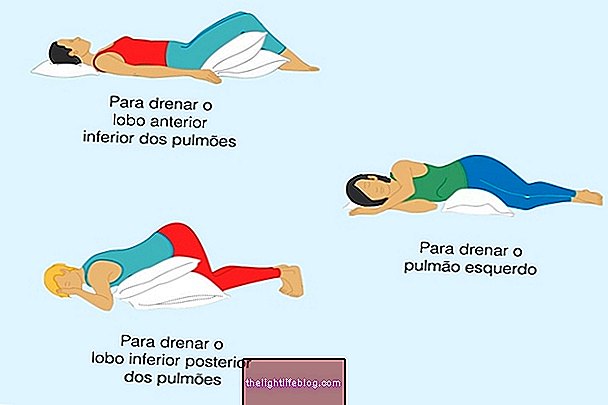
If it is the case of a bedridden person, here's how to position the person on the bed:

4. How to assess the risk of new ulcers
People who develop a pressure ulcer are at an increased risk of developing new ulcers. For this reason, it is advisable to assess the risk of having a new ulcer, which can be done using the Braden scale.
The Braden scale evaluates 6 factors that can contribute to the appearance of an ulcer and which include: the person's ability to feel pain, skin moisture, the level of physical activity, the ability to move, the nutritional status and the possibility there is friction on the skin. A value ranging from 1 to 4 is assigned to each of these factors, and at the end all values must be added to obtain the risk classification of developing a pressure ulcer:
- Less than 17: no risk;
- 15 to 16: mild risk;
- 12 to 14: moderate risk;
- Less than 11: high risk.
According to the risk, as well as the factors with the lowest score, it is possible to create a care plan that helps to prevent a new ulcer, in addition to facilitating the healing of the existing one. Some cares may involve hydrating the skin properly, encouraging a more adequate diet or stimulating physical activity, even if moderate.
Was this information helpful?
Yes No
Your opinion is important! Write here how we can improve our text:
Any questions? Click here to be answered.
Email in which you want to receive a reply:
Check the confirmation email we sent you.
Your name:
Reason for visit:
--- Choose your reason --- DiseaseLive betterHelp another personGain knowledge
Are you a health professional?
NoMedicalPharmaceuticalsNurseNutritionistBiomedicalPhysiotherapistBeauticianOther
Bibliography
- AMERICAN COLLEGE OF SURGEONS. Wound Home Skills Kit: Pressure Ulcers. 2018. Available at:. Accessed on 10 Jul 2019
- UNIVERSITY HOSPITAL OF SOUTHAMPTON - NHS. How to prevent pressure ulcers: information for patients, families and carers. 2017. Available at:. Accessed on 10 Jul 2019
- MUNICIPAL HEALTH SECRETARIAT - FLORIANÓPOLIS MAYOR. Wound Care Protocol. 2008. Available at:. Accessed on 10 Jul 2019
- PEREIRA, Cândida. Continuous quality improvement program: prevention of pressure ulcers. 2014. Curral das Freiras Health Center.
- DGS. Guidance from the Directorate-General for Health: Braden Scale - Adult and pediatric version. 2011. Available at:. Accessed on 10 Jul 2019
.jpg)