Gonorrhea is knee osteoarthritis, common in people over 65 years of age, although the most affected are women during menopause, which is usually caused by some direct trauma, such as a fall in which the person falls with the knees on the floor, for example.
Gonorrhea can be classified as:
- Unilateral - when it only affects 1 knee
- Bilateral - when it affects the 2 knees
- Primary - when you can not find its cause
- Secondary - when it is caused by overweight, direct trauma, dislocation or fracture, for example.
- With osteophytes - when small bony callus appears around the joint
- With reduction of the intra-articular space, which allows the femur and the tibia to touch themselves causing intense pain;
- With subchondral sclerosis, which is when there is degeneration or deformity of the tip of the femur or the tibia, inside the knee.
Gonorrhea does not always have a cure, but it is possible to decrease pain, increase the range of movements, improve the quality of life and well-being of the patient with the treatment that can be done with analgesic and anti-inflammatory drugs and with daily sessions of physiotherapy, which should be started as soon as possible. The treatment time varies greatly from one individual to another, but will never be less than 2 months.
Best treatments for gonarthrosis
The grades of gonarthrosis, according to the classification of Kellgreen and Lawrenc, are in the following table:
| Characteristics of Gonarthrosis seen on the X-ray | Best treatment | |
| Grade 1 | Decreased small articular space, with possible osteophyte on edge | Weight loss + water aerobics or body building + anti-inflammatory ointments to apply at the pain site |
| Grade 2 | Possible narrowing of joint space and presence of osteophyte | Physiotherapy + anti-inflammatory and analgesic remedies |
| Grade 3 | Multiple joint osteophytes, subchondral sclerosis and deformity in the bone contour | Physiotherapy + remedies + Infiltration of corticosteoid in the knee |
| Grade 4 | Severe articular narrowing, severe subchondral sclerosis, deformity of the bone contour and several large osteophytes | Surgery to place prosthesis in the knee |
How is Physical Therapy for Gonorrhea
The physiotherapeutic treatment of gonarthrosis should be done in an individualized way because not always what is indicated for one patient serves the other. But some features that can be used are TENS, ultrasound and infrared, plus pockets of warm or cold water and exercises indicated by the physiotherapist.
Joint mobilization techniques and manipulation are also indicated because they increase the production of synovial fluid that irrigates the joint internally and decreases chronic pain. When the person has changes such as imbalance, poor posture and deviations from the knee in or out, exercises that improve posture and correct these deviations, such as global postural reeducation, for example, can be used.
The most indicated exercises are those of muscle strengthening with elastic bands or weights that can vary from 0.5 to 5 kg, depending on the degree of strength that the person has. Less weight and greater repetition are ideal for decreasing muscle stiffness and can be performed to strengthen the front, back and sides of the thigh. In conclusion, stretches can be made to the thigh. Here are some examples of exercises for knee arthrosis.
To help the person walk and move around in the home, crutches or walking sticks may be recommended to better distribute body weight, reducing pressure on the knees.
Gonartrose causes disability?
People with grade 3 or 4 gonarthrosis may have difficulty working due to constant pain and the inability to stand and hold weight, so when treatment with physical therapy, medications and surgery is not enough to return the quality of life and to enable the work already performed by the person, the person may be considered invalid and retire. But usually these degrees of gonarthrosis only happen in people over 65 when she is already retired.
Who is at greatest risk of having
Women are usually affected after age 45 and men after age 50, but virtually all older people over 75 suffer from knee osteoarthritis. It is believed that knee arthrosis may appear early before age 65 in the following situations:
- Women in menopause;
- People with osteoporosis;
- In case of lack of vitamin C and D;
- People who are overweight;
- People with diabetes or high cholesterol;
- People who have very weak thigh muscles;
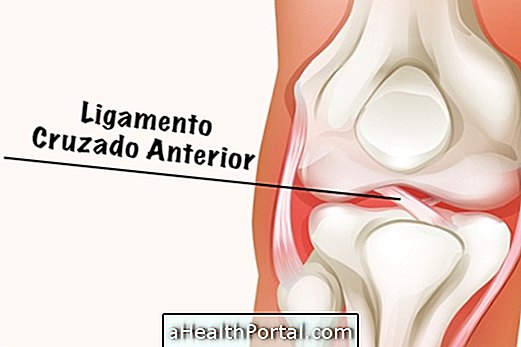
- In case of anterior cruciate ligament rupture or meniscus rupture in the knee;
- Changes such as genovaro or genovalgo, which is when the knees are facing in or out.
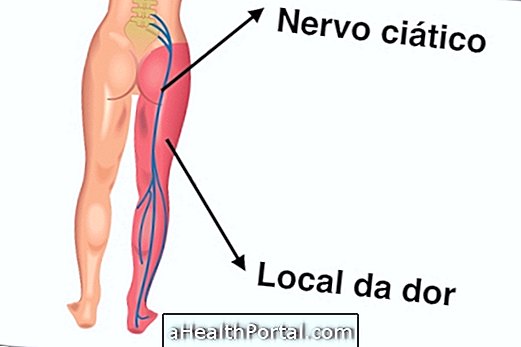
The symptoms of knee pain and creping can arise after a knee fall on the floor, for example. The pain usually arises when exerting some effort or doing physical activity, but in the most advanced cases it can remain for most of the day.
In people over the age of 65 the presence of small osteophytes, which can be seen on the knee X-ray, may indicate a greater severity of symptoms and need for treatment with physical therapy, and in more severe cases surgery to place a prosthesis on the knee may be indicated.