The liver is the organ most susceptible to the formation of abscesses, which may be solitary or multiple, and which may arise due to a spread of bacteria through the blood or the local dissemination of outbreaks of infection of the peritoneal cavity, near the liver, as is the case of appendicitis, diseases associated with biliary tract or pileflebite, for example.
In addition, hepatic abscess is a pathology that can also be caused by protozoa, known as amebic liver abscess.
Treatment depends on the body that is the source of the infection but usually consists of administration of antibiotics, drainage of the abscess or in more severe cases, it may be recommended to resort to surgery.

What are the signs and symptoms
The signs and symptoms that usually occur in people who have a liver abscess are fever, and in some people, especially those with disease associated with the biliary tract, may have signs and symptoms located in the upper right quadrant, such as abdominal pain.
In addition, chills, anorexia, weight loss, nausea and vomiting may also occur.
However, only about half of people with hepatic abscesses have enlarged liver, right upper quadrant palpation or jaundice, meaning that many people do not have symptoms that direct attention to the liver. Fever of obscure origin may be the only manifestation of the hepatic abscess, especially in the elderly.
Possible causes
Hepatic abscesses can be caused by different microorganisms, such as bacteria or even fungi, which may arise due to a spread of bacteria through the blood or the local dissemination of outbreaks of infection of the peritoneal cavity, near the liver, such as appendicitis, diseases associated with biliary tract or pileflebite, for example. Learn more about appendicitis and how you can identify it.
In addition, hepatic abscesses may also be amoebic:
Amebian liver abscess
The amebic liver abscess consists of a protozoal liver infection. The disease begins when E. histolytica protozoa penetrates through the intestinal mucosa, traverses the portal circulation and reaches the liver. Most of the patients with this disease do not present signs and symptoms nor the presence of the protozoa in the feces.
The disease can arise for months to years after a trip or residence in an endemic area, so it is important to know the careful history of the trip to make the diagnosis. The most common symptoms are pain in the upper right quadrant, fever and liver sensitivity.
The most common laboratory data are leukocytosis, elevated alkaline phosphatase, mild anemia and a high erythrocyte sedimentation rate.

What is the diagnosis
The only more reliable laboratory finding is elevation of serum alkaline phosphatase concentration, which is generally high in people with hepatic abscess. Bilirubin and aspartate aminotransferase in the blood, leukocytosis, anemia, and hypoalbuminemia may also occur in about half of the cases.
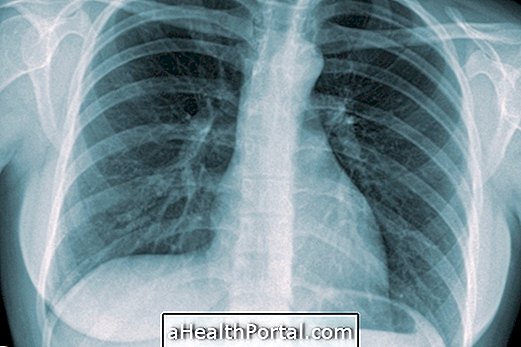
Imaging tests are usually the most reliable in the diagnosis of this disease, such as ultrasound, computed tomography, scintigraphy with indium or gallium labeled leukocytes and magnetic resonance imaging. An X-ray of the chest may also be performed.
The diagnosis of amebic liver abscess is based on the detection by ultrasonography or computed tomography of one or more lesions that occupy liver space and a positive serological test for antibodies to E. histolytica antigens .
How is the treatment done?
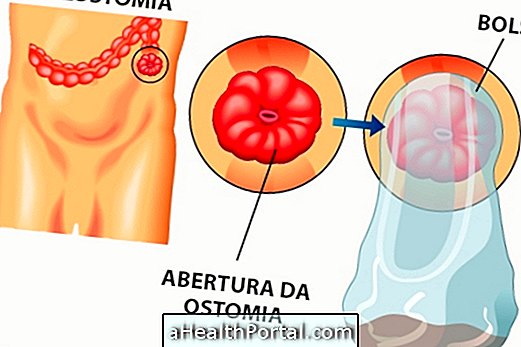
Treatment can be done by percutaneous drainage, with a catheter with lateral orifices kept in place. In addition, specific antibiotic remedies may also be used for the micro-organism responsible for the infection, after removal of a sample from the abscess. In cases where the abscess is drained, more time is required for antibiotic treatment.
If the infection is caused by candida, treatment usually consists of administration of amphotericin, with further treatment with fluconazole. In some cases, fluconazole treatment may be used only in clinically stable persons whose isolated micro-organism is susceptible to this drug.
For the treatment of amebic liver abscess, drugs such as nitroimidazole, tinidazole, and metronidazole may be used. To date, this protozoan has shown no resistance to any of these drugs. Drainage of amoebic liver abscesses is rarely necessary.