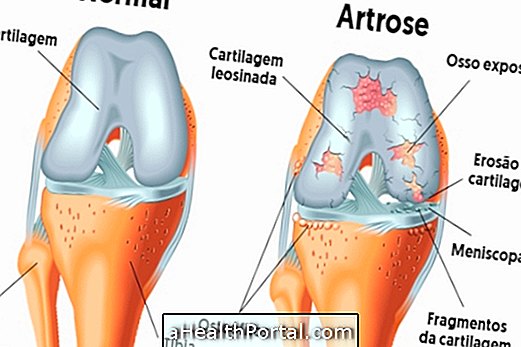
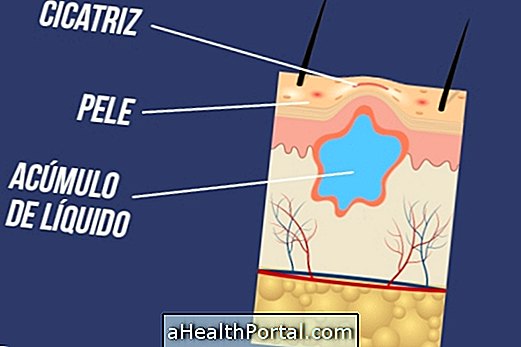
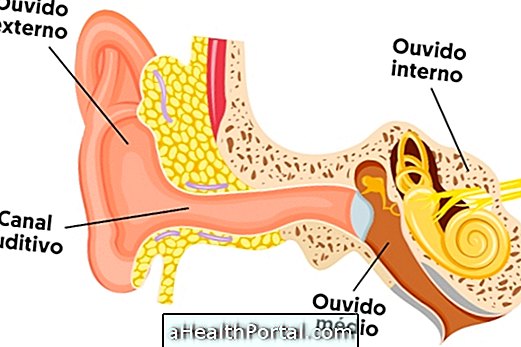
Synovitis is the inflammation of the synovial membrane, a tissue that lines the inner part of some joints, and therefore synovitis can occur in the foot, ankle, knee, hip, hand, wrist, elbow or shoulder.
In this disease the synovial membrane, which is responsible for producing the synovial fluid, becomes thicker and more blood vessels arise, which causes bleeding within the joint. This can happen due to a trauma, which may have been a fall or accident, or in some cases may arise as part of a disease such as rheumatism or gout. Overuse, as may happen during very repetitive work, in assembly plants, for example, does not cause synovitis, but aggravates its symptoms.

Types of synovitis
Synovitis can be classified by the orthopedic doctor as:
- Congenital synovitis: occurs when there is a small tissue called 'plica', which forms a fold inside the knee;
- Traumatic sinusitis: occurs after a fall, accident, twist, fracture or surgery;
- Rheumatoid Synovitis: is related to Rheumatoid Arthritis, or other diseases such as pigmented villyl node synovitis, crystalline synovitis, hemophilia or synovial chondromatosis;
- Infectious synovitis: occurs due to the presence of fungi or bacteria inside the joint.
Synovitis can still be classified as acute synovitis, when the symptoms have arisen shortly, and are related as an accident or fall, for example, and Chronic Synovitis, when symptoms have remained for more than 12 weeks, being related to diseases such as rheumatoid arthritis, for example.
Knee synovitis is one of the most common situations, causing pain, discomfort and swelling of the joint. See more on knee synovitis, popularly called 'knee water'.
How to know if it is Sinovite
Synovitis manifests itself through symptoms such as:
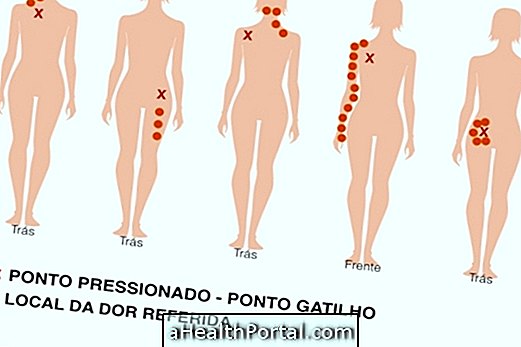
- Increased temperature in the joint, which can be felt by touch;
- Pain when moving the affected joint;
- Location may become more reddish;
- There may be a small local swelling;
- Difficulty in moving the joint and affected limb due to pain or swelling.
The doctor may come to the conclusion that the joint is inflamed by the symptoms presented, but only the joint puncture to remove a sample of the fluid can prove its severity, but x-ray and ultrasound may also be useful. Thus, the doctor usually asks for tests to confirm the disease, and indicates the taking of anti-inflammatory medicines for relief of symptoms. If symptoms persist for more than 15 days, compromising one's daily activities, physical therapy may be recommended.
Although anyone can develop a synovitis condition, this is more common in people with rheumatoid arthritis and juvenile rheumatoid arthritis, people who work with very repetitive movements, and sports people who train more than 1 hour a day for more than 5 days per week.

Treatments for synovitis
The first treatment option for a synovitis is resting the joint, and it is not always necessary to immobilize, it is enough for the person to be careful not to move the affected joint, sparing his effort. When synovial fluid is found to be altered, your doctor may do a puncture to remove this compromised fluid, aiding in a faster recovery.
To complement the treatment of synovitis one must do physiotherapy sessions, take anti-inflammatory medications and use anti-inflammatory ointments. In more severe cases, surgery called arthroscopy may be used to remove part of the synovial tissue.
Medicines
The remedies for synovitis may be the anti-inflammatory drugs like aspirin, ibuprofen, painkillers like paracetamol, and corticosteroids. Applying ointments with Diclofenac may also be an option for pain relief.
Cold compress
Putting a compress of cold water or ice on the affected joint is a great option to combat swelling and relieve pain.
Physiotherapy
Physical therapy can be performed, 2 or 3 times a week, containing cryotherapy, and equipment such as ultrasound, electrostimulation, laser and shortwave, for example. The treatment should be chosen by the physiotherapist himself after his personal evaluation. Mobilizing exercises and stretching can also be indicated. In the final phase of recovery, muscle strengthening exercises are recommended around the joint.
Puncture
The doctor may remove a portion of the synovial fluid to dislodge the joint, which provides good relief of symptoms and aid in recovery. However, this type of treatment is only indicated for the most severe cases, when the joint is very affected and swollen.
Application of corticosteroids
In addition to withdrawal of synovial fluid the doctor can give an injection directly into the joint containing corticoid, such as cortisone, a type of strong anti-inflammatory that brings relief of symptoms quickly.